If you're dealing with back pain, the first thing to know is that surgery is rarely the starting point. Almost all back pain cases get better with non surgical back pain treatments, which can be anything from simple at-home care to more advanced, minimally invasive procedures. This "conservative-first" philosophy is the standard way to manage both sudden injuries and those nagging chronic aches.
Exploring Your Path to Pain Relief Without Surgery
Trying to figure out back pain treatment can feel like you've been handed a map with no compass. The good news is that the path to relief is usually a logical journey that puts healing first, without jumping to invasive procedures.
Think of your options on a spectrum. On one end, you have the foundational stuff—lifestyle tweaks and specific exercises. Move a little further down, and you get into professional conservative care, like physical therapy and chiropractic adjustments.
For more stubborn pain, there are advanced interventional options. The key is getting a precise diagnosis. Understanding the why behind your pain is the critical first step that guides every decision after that, making sure you get the right care for your specific situation.
The Standard of Care: A Global Perspective
This focus on starting with conservative care isn't just a common practice; it's the globally recognized standard. In fact, the World Health Organization's first-ever guidelines on chronic low back pain recommend non-surgical approaches as the first line of defense in primary care settings worldwide. Their approach highlights a multi-faceted plan that often includes education, structured exercise, and physical therapies. You can read the full WHO guideline on chronic low back pain to see the global consensus for yourself.
This flowchart gives you a good visual of how non-surgical treatments typically progress, from the initial diagnosis to more advanced options if they're needed.
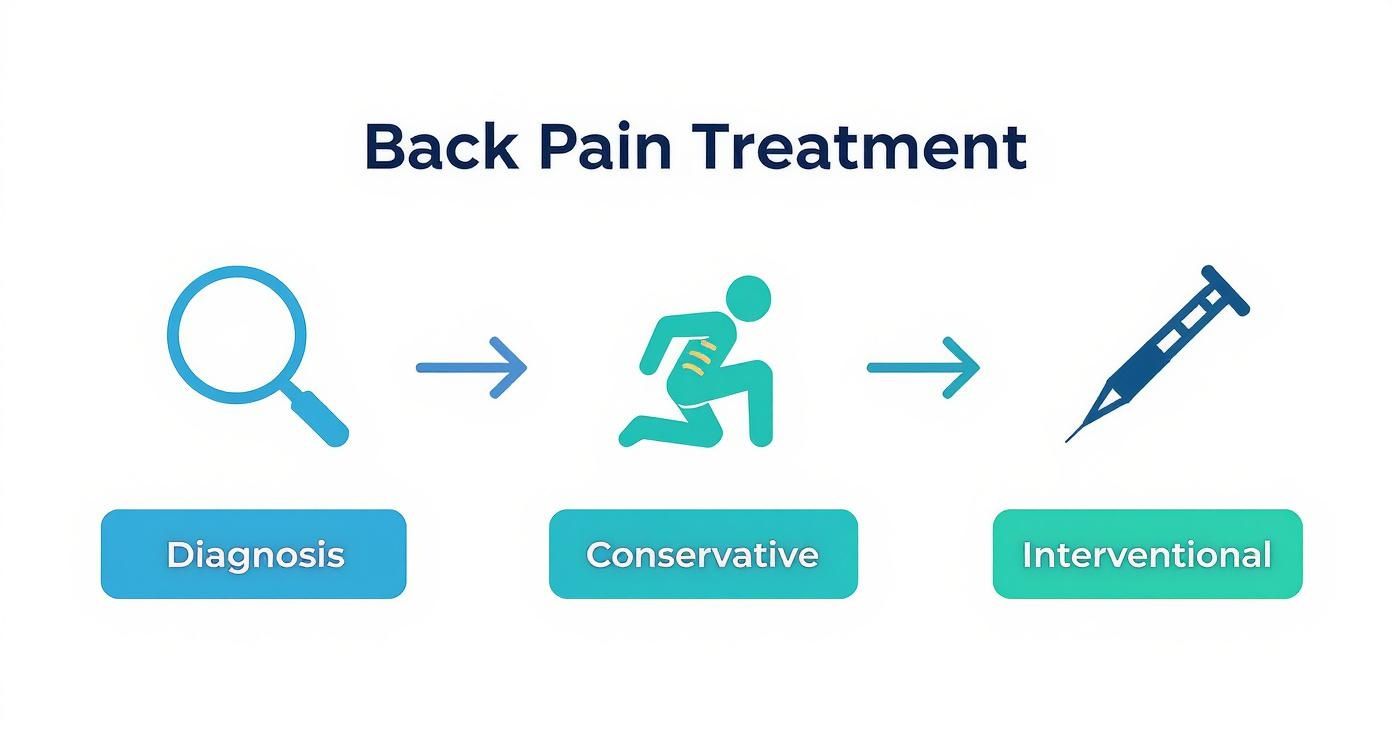
As you can see, it all starts with an accurate diagnosis. That's what guides the journey through conservative care and, only if necessary, into interventional therapies.
To give you a quick overview, here’s a simple breakdown of the main categories of non-surgical treatment.
Overview of Non Surgical Treatment Categories
| Treatment Category | Primary Goal | Common Examples |
|---|---|---|
| Conservative Care | Restore function and movement, reduce pain through manual therapy and exercise. | Chiropractic adjustments, physical therapy, targeted exercises, massage therapy. |
| Medications | Manage inflammation and acute pain to allow for participation in other therapies. | NSAIDs (ibuprofen), muscle relaxants, topical analgesics. |
| Interventional Procedures | Target specific pain generators with injections for diagnostic or therapeutic relief. | Epidural steroid injections, nerve blocks, radiofrequency ablation. |
| Regenerative Medicine | Stimulate the body's natural healing processes to repair damaged tissues. | Platelet-rich plasma (PRP) therapy, stem cell therapy. |
| Self-Care & Home Strategies | Empower you with daily habits to manage pain and prevent recurrence. | Ergonomic adjustments, heat/ice therapy, stretching, mindfulness. |
This table helps organize the options, but your provider will help you navigate which path is right for you.
Why Start with Conservative Treatments?
There's a good reason we don't just rush into surgery. Starting with less invasive methods works with your body's natural ability to heal and offers some major benefits. The whole philosophy is about helping your body repair and strengthen itself.
The goal of non-surgical care is not just to mask symptoms. It’s to address the underlying mechanical issues, improve function, and give you the tools to prevent pain from coming back. It’s about building a resilient foundation for long-term spinal health.
This approach gives you several key advantages:
- Lower Risk: Conservative options have minimal risks, especially when compared to the potential complications of surgery and anesthesia.
- Focus on Root Causes: Therapies like physical therapy and chiropractic care work to correct the biomechanical problems causing the pain, not just chase the symptoms.
- Empowers You: You become an active partner in your own recovery through exercises, ergonomic changes, and self-care. To dig deeper into this, check out our guide on how to manage chronic pain.
By trying these routes first, many people find lasting relief and completely avoid the need for more aggressive procedures. This guide will walk you through these options, step by step.
Building Your Foundation with Conservative Care
Lasting relief from back pain isn’t about quick fixes; it’s about building a strong, stable foundation for your spine. This is exactly what conservative care does. These are the essential, non-surgical treatments that anchor almost every successful recovery plan.
Think of it like building a house. A physical therapist is your architect, creating a custom blueprint of stretches and exercises designed just for you. Your chiropractor acts as the structural engineer, focusing on precise spinal alignment and making sure every joint moves correctly.
Then, your personal exercise routine becomes the daily maintenance crew, consistently working to keep everything strong, flexible, and ready for whatever life throws at it. These therapies don’t just mask symptoms—they work together to fix the root cause of the pain.

The Role of Physical Therapy
Physical therapy (PT) is a true cornerstone of treating back pain without surgery. A physical therapist is a movement expert who dives deep into your specific condition to build a program that improves your mobility, dials down the pain, and gets you back to doing what you love. The entire goal is active recovery—teaching you how to move your body safely and effectively again.
A good PT program is never one-size-fits-all. It usually includes a smart mix of passive and active treatments. Passive care, like heat or hands-on manual therapy, helps calm things down and get your body ready for movement. The active treatments are the specific exercises you do to build back strength and flexibility right where you need it most.
Physical therapy isn’t just about doing exercises in a clinic. It's about education. A good therapist empowers you with the knowledge to understand your body, manage your symptoms, and prevent future injuries long after your sessions have ended.
Chiropractic Care for Spinal Health
While PT gets your muscles and movement patterns on track, chiropractic care hones in on your nervous system and the mechanics of your spine. Chiropractors use precise, gentle adjustments to correct misalignments, often called subluxations. These adjustments are all about restoring proper joint motion and taking pressure off delicate nerves.
By improving the relationship between your spine and nervous system, chiropractic care helps unleash your body's natural ability to heal. For so many people, this leads to a huge drop in pain, better range of motion, and just feeling better overall. It’s a key piece of the puzzle when it comes to non-surgical back pain treatments.
We often use specialized techniques depending on who we're helping. For example, expecting mothers often find relief with the Webster Technique, which focuses on balancing the pelvis. For others, a gentle, instrument-based method like the Torque Release Technique (TRT) provides incredibly precise adjustments with minimal force.
The Power of Targeted Exercise
Both physical therapy and chiropractic care set the stage for the most important part of long-term back health: consistent, targeted exercise. We’re not talking about generic gym workouts here; this is a specific routine designed to support and protect your spine.
The main focus is almost always on strengthening your core—the web of muscles in your abdomen and back that acts like a natural corset for your spine. A strong core provides stability, takes the load off your spinal discs, and helps you maintain good posture without even thinking about it. To build that solid foundation, it’s vital to understand how to strengthen core muscles the right way.
A great program will always include:
- Core Strengthening: Moves like planks, bird-dogs, and bridges that stabilize your entire torso.
- Flexibility and Mobility: Stretches for tight spots like the hamstrings, hip flexors, and lower back to improve how you move.
- Low-Impact Aerobics: Things like walking, swimming, or cycling that boost blood flow to healing tissues without jarring your spine.
These three pillars—physical therapy, chiropractic care, and targeted exercise—are a powerful team. PT builds functional strength, chiropractic ensures optimal alignment, and your daily exercise routine locks in those gains for lasting relief and resilience.
Understanding the Role of Pain Management Medications
When your back flares up, reaching for medication can feel like the fastest way to get relief. And while it’s a valuable tool, I always encourage my patients to think of it as a temporary bridge, not the final destination.
The real job of pain medication is to dial down the pain and inflammation just enough so you can actively participate in the therapies that fix the underlying problem—things like physical therapy, targeted exercises, or chiropractic care.
Think of it this way: medication can quiet the alarm bells (the pain), but it can't fix what's causing the alarm to go off in the first place. By turning down the volume, it gives your body a chance to heal and makes it possible to perform the movements that build long-term strength and stability. This strategy is essential for a successful recovery, allowing you to break the pain cycle and engage with treatments that offer a real, lasting solution.
Common Medication Options for Back Pain
When it comes to medication, most doctors will start with the safest, most effective options for short-term relief. These drugs work in different ways to tackle pain from multiple angles.
The two main categories you'll likely encounter are:
-
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These are usually the first line of defense. You'll recognize over-the-counter options like ibuprofen (Advil, Motrin) and naproxen (Aleve). They work by blocking the enzymes that cause inflammation and pain, which makes them particularly effective for acute pain from a muscle strain or a minor injury.
-
Muscle Relaxants: If your back pain involves a lot of muscle spasms and intense tightness, your doctor might prescribe a muscle relaxant. These medications work on your central nervous system to ease muscle tension and stop the painful cramping that often comes with back injuries.
It's crucial to use these medications exactly as directed to avoid potential side effects. Even over-the-counter drugs aren't without risks if they're used improperly or for too long.
The Limits of Medication
While helpful, medication alone has its limits. A massive analysis of over 300 randomized trials shed some light on the reality of non surgical back pain treatments: only about 10% of common therapies showed a clear benefit beyond a placebo. While the study did find moderate evidence supporting NSAIDs for acute pain, it’s a sobering reminder that many treatments offer modest benefits at best. You can discover more insights from the back pain treatment study to get the full picture.
This really highlights a critical point: relying only on pills is almost always a short-term game. It won't strengthen weak core muscles, fix poor posture, or improve your spinal alignment.
Medication can get you to the starting line, but it can't run the race for you. True, lasting relief comes from combining symptom management with active, restorative care that addresses the root cause of your pain.
Ultimately, medication is just one piece of the puzzle. It creates a window of opportunity where you feel well enough to build a more resilient back. The most successful recovery plans use medication as a supportive tool, not the main event. This allows you to fully commit to the physical therapies, exercises, and lifestyle changes that create durable, long-term health and stop the pain from coming back.
Exploring Advanced Interventional Treatments
It can be really discouraging when you’ve done everything right—physical therapy, chiropractic care, dedicated exercises—and the back pain just won't quit. But hitting this wall doesn't mean surgery is your only option. There's a whole world of advanced, minimally invasive procedures that sit squarely in the middle ground.
Think of these treatments as a precision strike rather than a full-scale assault. Instead of a generalized approach, these non surgical back pain treatments zero in on the specific, identifiable source of your pain, whether it’s an inflamed nerve root or a grumpy, arthritic joint. They represent the next logical step when the foundational care just isn't cutting it.
These procedures are typically handled by specialists like physiatrists or pain management doctors. They use sophisticated imaging tools, like live X-rays called fluoroscopy, to guide their instruments with incredible accuracy right to the trouble spot.
Precision Injections for Targeted Relief
One of the most common and effective interventional strategies is therapeutic injections. The goal here is simple: deliver a powerful anti-inflammatory medication directly to the source of the problem. This provides far more potent relief than any oral medication could.
Here are a few of the main types:
-
Epidural Steroid Injections (ESIs): This is a go-to for sciatica—that sharp, radiating pain down the leg. It’s usually caused by a herniated disc or spinal stenosis putting pressure on a nerve. A corticosteroid is injected into the epidural space around the spinal nerves to calm the inflammation and, in turn, the pain.
-
Facet Joint Injections: Your spine is stabilized by small, connecting joints called facet joints, which can become arthritic and painful over time. For this, a doctor injects a mix of local anesthetic and steroid right into the joint. It's a two-for-one: it helps diagnose the pain source and provides immediate relief.
-
Sacroiliac (SI) Joint Injections: The SI joint, which connects your spine to your pelvis, is a notorious and often overlooked source of low back pain. Much like a facet injection, this procedure targets the SI joint directly to reduce painful inflammation.
These injections can offer relief for several weeks or even months. More importantly, they create a crucial pain-free window, allowing you to finally make real progress with physical therapy and strengthening exercises.
To help you keep these straight, here is a quick comparison of the most common interventional procedures.
Comparing Interventional Back Pain Treatments
This table breaks down some of the most common procedures, helping you understand their purpose, what they're used for, and how long you can typically expect the relief to last.
| Procedure | Targets This Condition | How It Works | Typical Relief Duration |
|---|---|---|---|
| Epidural Steroid Injection (ESI) | Sciatica from Herniated Disc or Spinal Stenosis | Injects anti-inflammatory medication into the epidural space to calm nerve irritation. | Weeks to several months |
| Facet Joint Injection | Arthritis or inflammation in the small stabilizing joints of the spine. | Injects anesthetic and steroid directly into the joint to diagnose and relieve pain. | Weeks to several months |
| Sacroiliac (SI) Joint Injection | Pain and inflammation in the joint connecting the spine and pelvis. | Injects anesthetic and steroid into the SI joint to reduce inflammation. | Weeks to several months |
| Radiofrequency Ablation (RFA) | Chronic pain from arthritic facet joints confirmed by a diagnostic block. | Uses heat from a radiofrequency current to "turn off" specific pain-sending nerves. | 6 to 18 months |
Each of these serves a different purpose, and a pain specialist can help determine if one is the right fit for your specific condition.
Radiofrequency Ablation for Longer-Lasting Results
For stubborn pain coming from arthritic facet joints, Radiofrequency Ablation (RFA) can be a game-changer. If you get good, temporary relief from a facet joint injection, you might be a great candidate for this longer-lasting solution. Think of it as hitting the "pause button" on a very specific pain signal.
It starts with a diagnostic nerve block to confirm exactly which nerves are sending the pain signals from that arthritic joint. If that test works, you move on to RFA.
During the procedure, a specialized needle is guided to that target nerve. A radiofrequency current is then sent through the needle, creating a tiny, precise heat lesion. This doesn't damage the joint itself; it just interrupts the nerve’s ability to tell your brain that it hurts.
The beauty of Radiofrequency Ablation is its specificity. It doesn't fix the underlying arthritis, but by selectively turning off the pain signal from that joint, it can provide relief that often lasts for 6 to 18 months, allowing you to live and move more comfortably.
The Emerging Field of Regenerative Medicine
A newer and exciting frontier in non-surgical care is regenerative medicine. The core idea is to harness your body's own powerful healing abilities to repair damaged tissue. While the science is still evolving, these treatments are showing real promise for certain back conditions.
Two of the most common options you’ll hear about are:
-
Platelet-Rich Plasma (PRP) Therapy: A small amount of your own blood is drawn and spun in a centrifuge. This process concentrates the platelets, which are packed with natural growth factors. This "liquid gold" is then injected into the injured area—like a damaged disc or joint—to kickstart the healing process.
-
Stem Cell Therapy: This procedure uses your body's own "master cells" to rebuild damaged tissue. Stem cells are typically harvested from your bone marrow or fat tissue and then injected into the site of injury, with the goal of helping regenerate cartilage or other structures. You can learn more about the specifics of stem cell therapy for pain in our detailed guide.
It’s important to go into regenerative medicine with realistic expectations. The evidence is still growing, and these treatments aren't yet a standard of care for every back problem. But for the right person, they offer a unique way to stimulate the body's own repair crew and promote genuine healing.
The Power of Lifestyle and Self-Care Strategies
Professional treatments are a vital part of recovering from back pain, but what you do day-to-day is what makes that progress stick. It helps to think of your chiropractor or physical therapist as a coach drawing up the plays. Your daily habits—how you move, sit, eat, and handle stress—are how you actually run those plays and win the game against pain.
These everyday choices are the bedrock of long-term spinal health. They’re what turn temporary relief into lasting strength, putting you back in control. When you build a spine-friendly lifestyle, you create a body that’s less likely to get injured and better equipped to heal when it does.

Creating Your Spine-Friendly Environment
Your surroundings can either be a partner in your recovery or an obstacle. Making a few small, deliberate changes to your environment can take a surprising amount of strain off your spine. This is especially important at your workspace, where many of us log thousands of hours every year.
An ergonomic setup isn’t a perk; it’s a must-have for preventing chronic pain. And thankfully, simple tweaks make a huge difference.
- Adjust Your Chair: Your feet should rest flat on the floor, with your knees bent at about a 90-degree angle. Make sure your lower back feels supported—grab a lumbar pillow if your chair falls short.
- Position Your Monitor: The top of your screen should be at or just below eye level. This simple fix prevents that forward-head slouch that strains your neck and upper back.
- Master Proper Lifting: When lifting, always bend at your knees, not your waist. Keep the object tucked in close to your body and tighten your core muscles to shield your lower back from the load.
These aren't just one-time adjustments. They’re new habits that actively protect your spine all day long.
Fueling Your Body to Reduce Inflammation
What you eat directly affects your body’s inflammation levels, a key driver behind most pain. Following an anti-inflammatory diet can be a powerful non surgical back pain treatment that works from the inside out. It’s not about cutting things out, but about crowding your plate with foods that support your body’s natural healing abilities.
Think of food as medicine. Nutrient-dense, anti-inflammatory foods provide the raw materials your body needs to repair tissue, calm irritation, and reduce pain signals.
Try to weave more of these foods into your meals:
- Omega-3 Fatty Acids: Found in salmon, walnuts, and flaxseeds, these healthy fats are proven inflammation fighters.
- Leafy Greens: Spinach, kale, and other greens are loaded with antioxidants that protect your cells from stress and damage.
- Colorful Fruits: Berries, cherries, and oranges are full of compounds that help lower inflammatory markers in the body.
On the flip side, try to limit processed foods, sugary drinks, and refined carbs. These can promote inflammation and work against all your recovery efforts.
The Mind-Body Connection in Pain Relief
Back pain is never just a physical problem; it has a huge mental and emotional impact. Practices like yoga and mindfulness are proven to not only reduce muscle tension but, more importantly, change how you relate to pain. They teach you to respond to discomfort with calm awareness instead of instinctual fear and tightening.
Gentle yoga improves flexibility, strengthens your core, and encourages deep relaxation. At the same time, mindfulness meditation can help quiet a nervous system that has become overactive from dealing with chronic pain. Studies have even shown that just a few minutes of mindfulness a day can significantly lower how much pain you feel. By bringing these practices into your routine, you’re addressing both body and mind for a much more complete path to healing.
How to Find the Right Professional for Your Back Pain
Figuring out who to see when your back hurts can feel like a maze. Honestly, knowing who to call is the first, and most important, step toward getting real relief with non surgical back pain treatments. Your journey should always start with a professional who can give you a clear, accurate diagnosis.
Your primary care provider (PCP) is the perfect person to see first. They can make sure nothing serious is going on, help you manage the initial pain, and point you toward the right specialist. Think of your PCP as your trusted guide—they have the map and can show you the best path forward.
For most people, that path leads to a specialist focused on conservative, hands-on care. These are the experts in getting you moving again without jumping straight to invasive procedures.
Who Should Be on Your Care Team
Depending on what’s causing your pain, your care team might have a few different experts, each playing a unique role in your recovery.
- Physiatrist (PM&R Doctor): These doctors are non-surgical spine specialists. They are experts at diagnosing and treating muscle and joint conditions with tools like physical therapy and precisely targeted injections. They’re fantastic at building a big-picture, conservative treatment plan.
- Physical Therapist (PT): A PT is a movement expert. They’ll create a personalized exercise program to rebuild your strength, get your flexibility back, and, most importantly, teach you how to move safely to keep the pain from coming back.
- Chiropractor: A chiropractor is a specialist who focuses on the mechanics of your spine and how it connects to your nervous system. They use skilled manual adjustments to restore proper movement in your joints and take pressure off nerves.
- Pain Management Specialist: This is usually an anesthesiologist or physiatrist who is an expert in more advanced interventional options, like epidural steroid injections or radiofrequency ablation, for pain that just won’t quit.
It’s a huge plus when you can find a team that works together. When a physiatrist can walk down the hall to chat with a physical therapist or chiropractor about your progress, you get a plan that’s truly tailored to you.
Key Questions to Ask Any Provider
Finding a provider you click with and trust is everything. Before you agree to any treatment plan, don't hesitate to ask some questions to make sure you’re on the same page. It’s your body, and you should be an active partner in your own care.
A great healthcare provider doesn't just treat your symptoms; they empower you with knowledge. They should be willing to explain your condition, discuss all available options, and work with you to set realistic goals for your recovery.
Here are a few essential questions to get the conversation started:
- What is your overall philosophy for treating back pain? Do you always start with conservative care?
- For a condition like mine, what specific techniques or therapies do you typically use?
- How will we track my progress, and what’s our plan B if the first approach doesn't work?
- Do you have experience treating patients with unique needs, like prenatal or pediatric back pain?
By asking these simple questions, you can find a professional whose approach aligns with your own goals. The right partner will give you the confidence you need to walk the path to recovery and find lasting relief without surgery.
Common Questions About Non-Surgical Back Pain Treatments
When you're trying to find your way out of back pain, it’s only natural to have a lot of questions. Getting clear, straightforward answers can make you feel more confident and in control of your recovery. Let’s tackle some of the most common things people wonder about when they start exploring their options.
How Long Should I Try Non-Surgical Treatments?
This is probably the most important question people ask, and the answer really comes down to one word: consistency. Most experts agree you should commit to a dedicated course of conservative care for at least 6 to 12 weeks before even considering more invasive options like surgery.
For many chronic conditions, that timeframe can easily stretch to six months or even longer. The key isn't just to let time pass, but to actively engage with your plan—whether it's physical therapy, chiropractic care, or a specific exercise routine. If your pain isn’t getting better after that dedicated period, or if you notice scary new symptoms like progressive weakness in your legs, it’s time to have a serious talk with your doctor about what’s next.
Are Complementary Therapies Like Massage Effective?
Things like massage and acupuncture can be fantastic additions to a recovery plan, but how well they work is often very individual. While some big scientific studies show mixed results, countless people will tell you they’ve found significant relief with these therapies.
Even the World Health Organization (WHO) recognizes massage as a potential part of physical therapy. These approaches are generally very safe and are wonderful for easing muscle tension, improving circulation, and just helping you feel better overall. They tend to work best when they're part of a bigger plan that also includes active treatments, like targeted exercises, to fix the root mechanical problems.
Think of complementary therapies as powerful supporting actors. They might not be the star of the show, but they can make the entire production—your recovery—run a whole lot smoother.
Can Non-Surgical Treatments Provide a Permanent Cure?
Whether a "cure" is on the table often depends on the type of back pain you have. For acute pain from a simple muscle strain, absolutely. The right non-surgical treatments can lead to a complete and permanent recovery.
However, for chronic back pain tied to long-term conditions like degenerative disc disease or arthritis, the goal shifts from a "cure" to effective, long-term management. In these situations, successful non-surgical back pain treatments are designed to:
- Significantly lower your pain levels
- Dramatically improve your ability to move and function day-to-day
- Give you the tools (like exercises and ergonomic habits) to manage flare-ups on your own
The ultimate goal is to put you back in control, so your condition no longer dictates how you live your life. It’s all about getting you back to the activities you love with confidence and strength.
At First Steps Chiropractic, we specialize in creating personalized, non-surgical care plans for the entire family. If you're ready to find the root cause of your back pain and take control of your health, we invite you to book a complimentary consultation with our team. Explore your options with us at https://firststepschiropractic.com.

