When you’re dealing with chronic pain, it often feels like you’re fighting a battle on multiple fronts. It’s not just a physical ache; it’s a constant drain that affects your mood, your work, and your relationships. Real, lasting relief rarely comes from a single pill or a one-off treatment. Instead, it’s about building a well-rounded strategy that tackles the pain from every angle, weaving together movement, mindset, and lifestyle adjustments to genuinely get your life back.
Your First Step in Managing Chronic Pain
If you've been living with pain that just won't go away, you know it's so much more than a physical symptom. It’s the frustration of feeling stuck, the exhaustion from sleepless nights, and the disappointment of missing out on life. The most important thing to realize right now is that this isn't just "your life" now. Taking back control is absolutely possible, and you're not on this journey alone.
We define chronic pain as any pain that hangs around or keeps coming back for more than three months. This isn't the same as acute pain, like when you sprain your ankle. Acute pain is your body’s alarm system—it signals an injury and fades as you heal. Chronic pain is different. The alarm keeps blaring long after the initial problem has healed, or sometimes, it starts without any clear reason at all.
Shifting Your Perspective on Pain
One of the biggest traps people fall into is treating chronic pain like it's a simple injury, constantly searching for that one magic bullet to "fix" it. I’ve seen this lead to so much frustration over the years. The truth is, managing long-term pain requires a shift in mindset. It’s less about making the pain disappear completely and more about turning down its volume so it no longer runs your life.
This journey starts by assembling your personal pain management toolkit. Think of it like a toolbox where every tool has a unique and vital job to do.
The International Association for the Study of Pain defines pain as “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.” This really gets to the heart of it: pain is as much an emotional event as it is a physical one.
Understanding the Scale and Scope
It can feel isolating, but recognizing just how many people are in the same boat can be incredibly validating. This isn’t some rare, personal failing; it's a massive global health issue. Millions of people are navigating this, which means there’s a huge push for better solutions.
The global chronic pain market was valued at nearly US$ 79.96 billion in 2024 and is expected to keep growing. This isn't just a number—it shows that more awareness and research are being poured into finding effective strategies. You can find more details on this trend over at marketresearch.com.
What this really means for you is hope. More resources are being dedicated to helping people just like you find meaningful relief.
Building Your Foundational Roadmap
Your path to feeling better will be uniquely yours, but the most successful plans I’ve seen all draw from a few core areas. The goal isn't just to cover up symptoms but to get to the root of what’s keeping that pain cycle going. Your plan should be a living, breathing thing that you can adjust as your needs change.
A solid pain management plan usually includes:
- Physical Therapies: Think gentle movement, targeted exercises, and chiropractic care. The focus is on improving strength and flexibility without triggering a flare-up.
- Mental Health Strategies: Techniques like mindfulness and Cognitive Behavioral Therapy (CBT) are powerful tools. They help you reframe the negative thoughts that often come with pain and reduce its emotional toll.
- Lifestyle Adjustments: This is about the small, daily choices that add up. An anti-inflammatory diet, better sleep habits, and learning to pace your activities can make a world of difference in your energy levels and pain.
Consider this guide your starting point—a resource to help you pull these strategies together, build your resilience, and start truly living again.
Building Your Physical Foundation for Pain Relief
When you live with constant pain, the thought of exercise can be terrifying. I see it all the time in my practice—the fear that any movement will trigger a flare-up is very real. It’s a vicious cycle. People become less active to avoid pain, which ironically leads to more stiffness and discomfort over time.
The secret is to completely reframe what "activity" means. We're not talking about running a marathon or hitting a high-intensity gym class. It’s about gentle, consistent movement that reassures your body it’s safe to be flexible and strong again.
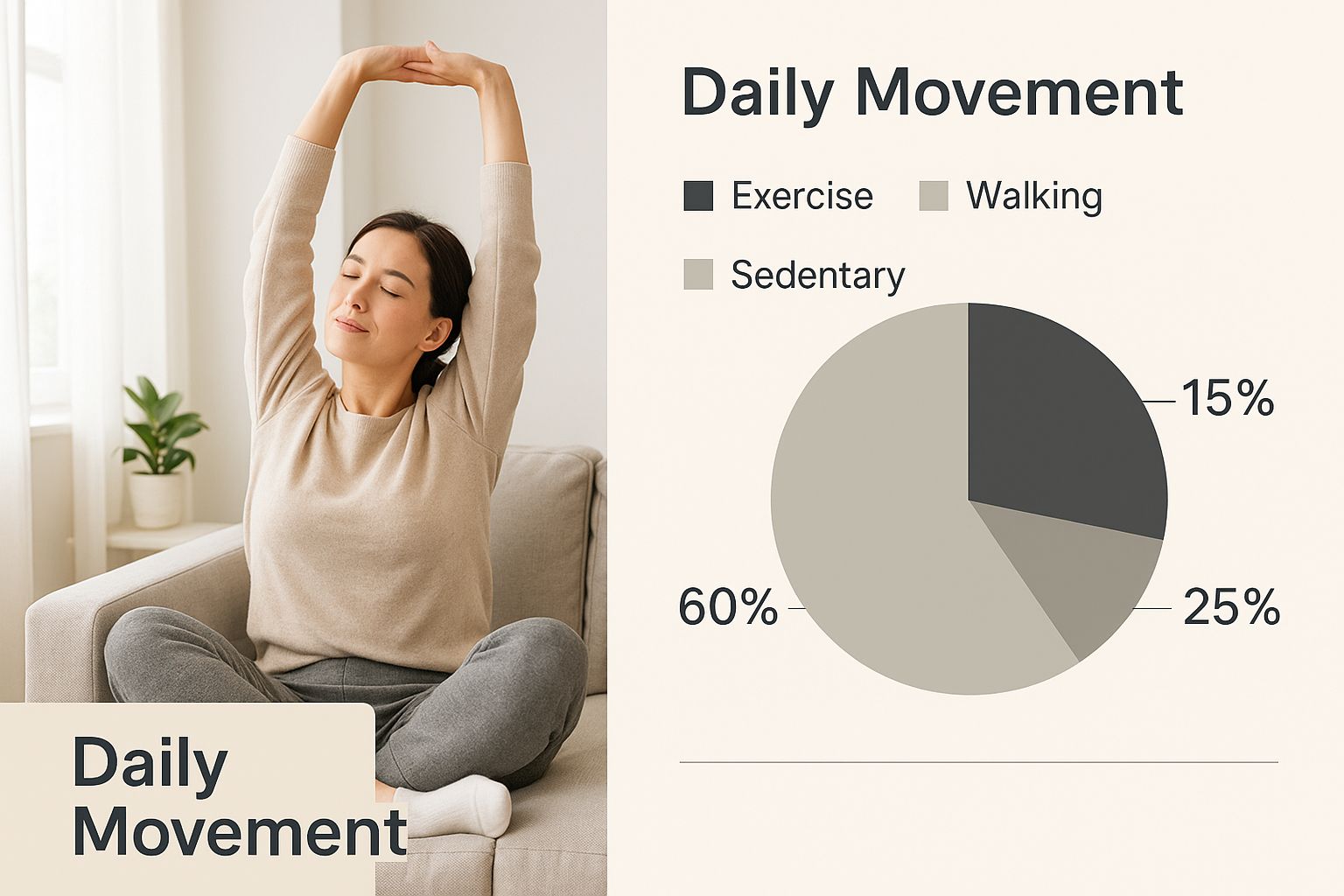
As you can see, the journey to relief starts small. It begins with simple, sustainable actions you can do right from the comfort and safety of your own home.
Moving Beyond the Fear of Movement
That first step is almost always the hardest. It’s a mental hurdle—committing to move your body in a way that feels supportive, not punishing. The real goal here is to unlock your body's own natural painkillers, known as endorphins, while gently coaxing back your range of motion.
For so many, this is a monumental challenge. The numbers back this up. In 2023, about 24.3% of adults in the United States dealt with chronic pain, and 8.5% faced pain so severe it significantly limited their daily lives. You can dig into the CDC data brief on chronic pain prevalence to see the full picture. These aren't just statistics; they represent millions of people searching for a way to regain function and improve their quality of life.
Your journey has to start with choosing movements that build you up, not break you down.
Exploring Gentle Movement Therapies
Not all exercise is created equal, particularly when chronic pain is in the picture. High-impact activities can be jarring and counterproductive. Instead, we turn to low-impact disciplines celebrated for their ability to build strength and flexibility without adding strain.
A few powerful options I often recommend include:
- Restorative Yoga: This isn't your typical power yoga class. It uses props like blankets and bolsters to completely support your body in gentle, relaxing poses. The focus is on deep relaxation, releasing stubborn muscle tension, and calming the nervous system.
- Tai Chi: People often call this "meditation in motion," and for good reason. It involves slow, flowing movements that dramatically improve balance, flexibility, and your awareness of your own body. It's an incredible tool for reducing stiffness and preventing falls.
- Aquatic Therapy: For many, exercising in a warm pool is a complete game-changer. The water’s natural buoyancy supports your body weight, taking immense pressure off of painful joints. At the same time, it provides gentle resistance to help you build muscle strength safely.
To help you decide which approach might be right for you, I've put together a simple comparison.
Comparing Gentle Movement Therapies for Chronic Pain
This table breaks down some of the most common low-impact therapies, highlighting their benefits and who they're best suited for.
| Therapy Type | Primary Benefits | Best Suited For | Getting Started Tip |
|---|---|---|---|
| Restorative Yoga | Reduces stress, releases muscle tension, calms the nervous system. | Individuals with high stress, muscle tightness, or anxiety related to pain. | Find a class specifically labeled "restorative" or "gentle" and let the instructor know about your pain. |
| Tai Chi | Improves balance, enhances flexibility, increases body awareness. | Older adults, those with balance issues, or anyone seeking a mindful movement practice. | Look for a beginner's class or follow a reputable online video to learn the basic forms at your own pace. |
| Aquatic Therapy | Builds strength with low impact, relieves joint pressure, improves mobility. | People with arthritis, fibromyalgia, or significant joint pain that makes land-based exercise difficult. | Check with local community centers or physical therapy clinics for warm-water pool therapy programs. |
Choosing the right therapy is a personal decision, but the goal is always the same: find a movement you enjoy and can stick with.
The most important rule when moving with chronic pain is to listen to your body. The old "no pain, no gain" motto absolutely does not apply here. If something sharply increases your pain, it’s a clear signal to pull back, not push through.
Partnering with a Physical Therapist
While you can certainly start this journey on your own, working with a physical therapist can be an invaluable asset. Think of them less as a drill sergeant and more as a personal coach for your body's mechanics. A good PT who specializes in chronic pain will work with you to design a plan that fits your unique needs.
They can help you:
- Identify and Correct Imbalances: They are experts at pinpointing weak muscles or faulty movement patterns that are contributing to your pain.
- Learn to Pace Yourself: They can teach you how to find the sweet spot between activity and rest, helping you avoid the classic "boom-bust" cycle of overdoing it and then crashing for days.
- Build Confidence: A therapist provides expert guidance and reassurance, which is crucial for overcoming the fear of movement and learning to trust your body again.
Physical therapy isn't just about getting short-term fixes. It's about learning lifelong skills to improve your daily function. It empowers you to take an active role in your own recovery, building a solid physical foundation for a life with less pain.
Mastering the Mind-Body Connection to Reduce Pain
Chronic pain isn't just happening in your back, neck, or joints. It’s a complex experience that your brain processes, interprets, and—all too often—amplifies. Grasping this critical mind-body link is a complete game-changer when it comes to managing chronic pain. It hands you a powerful new set of controls to work with.

Every single day, your brain sifts through countless signals from your body. But when you live with chronic pain, it’s like the "volume" knob for those pain signals gets cranked up and stuck on high. Feelings like stress, frustration, and anxiety don't just exist alongside the pain; they can physically make it worse, locking you into a vicious cycle that feels impossible to break.
This isn't just a theory; it's a well-documented reality. We've seen how pain can worsen psychological distress, which in turn makes the pain feel even more intense. It's a two-way street. Recognizing that this cycle is happening is the very first step to taking it apart, piece by piece.
Rewiring Your Brain with Cognitive Behavioral Therapy
One of the most effective, evidence-based tools for breaking this pain cycle is Cognitive Behavioral Therapy (CBT). This isn't just about talking; it's a practical, skills-based approach that teaches you how to spot, challenge, and ultimately reframe the negative thought patterns that are pouring fuel on your pain.
Think about it. When you’re always in pain, it's incredibly easy to fall into thought traps like, "This is never going to get better," or "I can't do anything I used to enjoy." These thoughts aren't harmless—they trigger a real stress response in your body, tensing your muscles and making the pain feel even more overwhelming. CBT gives you the tools to catch these thoughts in the act.
A therapist who specializes in pain management can guide you through practical exercises to:
- Recognize the automatic negative thoughts that pop up about your pain.
- Challenge them by looking for real-world evidence that contradicts them.
- Replace them with more balanced, helpful thoughts. For instance, swapping "I can't do anything today" with, "I'm having a high-pain day, so I'll focus on gentle activities I can do."
This process isn’t about pretending you're not in pain. It’s about fundamentally changing your relationship with it, so it no longer has total control over your emotional state.
Key Insight: CBT for pain management isn't about convincing yourself the pain isn't real. It's about training your brain to stop catastrophizing the sensation, which can directly lower its perceived intensity and give you back a sense of control.
Finding Calm with Mindfulness and Meditation
While CBT helps you actively restructure your thoughts, mindfulness and meditation teach you to simply observe them without getting tangled up in judgment. These practices are incredibly powerful for turning down the "volume" of your pain.
When you meditate, you're not trying to force the pain to go away. Instead, you're gently training your attention to rest on something neutral, like the rhythm of your breath. This simple act helps create a bit of space between the raw physical sensation of pain and the emotional suffering that usually comes with it. You learn to notice the pain without being completely swept away by it.
Here’s a simple way you can start today:
- Find a quiet spot where you can sit or lie down comfortably.
- Gently close your eyes and bring your full attention to your breath.
- Just notice the sensation of the air moving in and out of your body.
- Your mind will wander. That’s okay. When it does, just gently guide your focus back to your breath without any frustration.
Try starting with just five minutes a day. Over time, this consistent practice can help rewire your brain's default response to pain signals, encouraging a state of calm and reducing that constant feeling of being on high alert. Many people I've worked with find that this mental relief also translates into very real physical relief. The connection is that strong, which is why we also explore how chiropractic care can help with anxiety and depression in our other patient guides.
Using Nutrition and Lifestyle to Fight Inflammation
Your daily habits are some of the most powerful—and most accessible—tools in your pain management toolkit. While therapies and mental strategies are crucial, the choices you make every day about what you eat, how you sleep, and when you rest lay the foundation for their success.
These habits directly impact inflammation, energy levels, and your body's overall resilience. Think of systemic inflammation as a low-level "fire" constantly burning inside your body, making pain feel much worse. The good news? What you eat can either fan those flames or help put them out. Honestly, learning how to manage chronic pain often starts right in your own kitchen.
Embracing an Anti-Inflammatory Diet
An anti-inflammatory diet isn't about extreme restrictions or complicated rules. It’s simply about shifting your focus toward whole, nutrient-dense foods more often. The goal is to nourish your body with the building blocks it needs to calm inflammation from the inside out.
I always tell my patients to start by focusing on what you can add to your plate, not what you need to take away. This positive mindset makes the change feel much more manageable and a lot less like a punishment.
A few powerhouse food groups to start with are:
- Fatty Fish: Salmon, mackerel, and sardines are packed with omega-3 fatty acids, which are famous for their potent anti-inflammatory effects.
- Leafy Greens: Think spinach, kale, and collard greens. They're rich in antioxidants and vitamins that fight cellular stress.
- Berries and Cherries: These fruits are loaded with compounds called anthocyanins—that’s what gives them their vibrant color and powerful inflammation-fighting properties.
- Nuts and Seeds: Almonds, walnuts, and chia seeds offer a fantastic mix of healthy fats, fiber, and anti-inflammatory compounds.
At the same time, it’s wise to cut back on foods known to promote inflammation. This means things like sugary drinks, refined carbs (white bread, pasta), fried foods, and highly processed snacks. You don't have to banish them forever, but making them a "sometimes" food can make a world of difference.
The Critical Role of Restorative Sleep
Pain and poor sleep get tangled up in a frustrating cycle. Pain makes it incredibly difficult to fall asleep and stay asleep. Then, that lack of quality sleep makes you more sensitive to pain the next day. Breaking this cycle is absolutely essential for any real pain management plan.
Improving your sleep hygiene—the habits and environment around your sleep—can help. For instance, try creating a consistent sleep schedule, even on weekends. This simple step helps regulate your body's internal clock.
Expert Tip: Create a relaxing pre-bedtime routine that signals to your body it's time to wind down. This could be reading a book (a real one, not on a screen!), taking a warm bath, or listening to calming music. The key is to avoid screens for at least an hour before bed. The blue light can interfere with melatonin production, your body's natural sleep hormone.
Learning the Art of Pacing
One of the biggest hurdles I see people with chronic pain face is the "boom-bust" cycle. You have a good day, so you push yourself to catch up on everything you've missed, only to crash for the next two days in a painful flare-up. It's an exhausting and demoralizing pattern.
The solution is a technique called pacing. Pacing is simply the art of balancing activity with rest. It’s about doing a little bit, then resting before you feel wiped out. This approach helps you build stamina and consistency without triggering that painful backlash.
Imagine you want to clean the kitchen. Instead of trying to power through it all at once, you might:
- Empty the dishwasher (then sit down and rest for 15 minutes).
- Wipe down the counters (then rest again).
- Sweep the floor (and call it a day, feeling accomplished).
This method allows you to get things done without paying for it later. It keeps your energy levels more stable and helps you finally break that all-or-nothing cycle.
These lifestyle adjustments are fundamental. They support the work you do with your care team and amplify the effects of other treatments. Advanced technologies can also play a role in calming this inflammation, and you can learn more about how SoftWave therapy promotes natural healing from our detailed guide. By combining smart daily habits with targeted therapies, you create a powerful, multi-faceted approach to reclaiming your life from pain.
Assembling Your Pain Management Care Team
Trying to navigate the world of chronic pain on your own is an uphill battle. I’ve seen time and again that the most successful outcomes happen when you build a supportive, multidisciplinary care team. Think of it as a group of trusted professionals, each looking at your pain from a different angle. This isn’t about just seeing more doctors; it's about creating a partnership where you are firmly in the driver's seat of your own health.

This team approach ensures all the different pieces of the pain puzzle—the biological, the psychological, and even the social factors—are considered. Your primary care physician often acts as the quarterback, but other specialists play essential roles in creating a truly well-rounded plan. When everyone collaborates, your experience is heard and addressed, leading to a much more effective strategy.
Becoming The CEO Of Your Health
To get the most out of your care, you have to make a mental shift from being a passive patient to an active leader. This means preparing for your appointments, learning how to communicate effectively, and keeping a close eye on your progress. Taking this proactive stance not only empowers you but also gives your team the clear, direct information they need to help you best.
Before you walk into any appointment, do a little homework. Don't just show up and hope you remember everything you wanted to say.
- Write Down Your Top 3 Concerns: Time with any practitioner is valuable and often limited. Knowing your top priorities ensures the most important things get covered first.
- List Your Questions: What are you wondering about? Think about your condition, treatment options, or potential side effects. There's truly no such thing as a "silly" question here.
- Track Your Symptoms: Keep a simple journal. Note your pain levels on a scale of 1-10, what makes it better or worse, and how different treatments are affecting you.
This simple bit of prep work can transform a routine check-up into a productive strategy session. It shows your team you're engaged and gives them concrete data to work with, moving the conversation beyond vague descriptions of how you feel.
Exploring Complementary And Supportive Therapies
Beyond your core medical team, a whole world of complementary therapies can offer significant relief and support. These approaches often focus on calming the nervous system, easing muscle tension, and boosting your overall sense of well-being. They work beautifully alongside conventional treatments to create a more complete and holistic approach to managing pain.
Many of our patients find tremendous value in adding these therapies to their routine:
- Acupuncture: This ancient practice involves inserting incredibly thin needles into specific points on the body. It’s believed to stimulate your body's own natural painkillers and improve energy flow, often providing real relief for chronic back pain, neck pain, and headaches.
- Massage Therapy: A skilled massage therapist can do wonders for releasing tight, knotted muscles, reducing stress, and improving circulation. From gentle Swedish massage to more intensive deep tissue work, the techniques can be tailored to your specific needs.
- Heat and Cold Therapy: This is one of the easiest and most accessible tools in your kit. A heating pad can relax stiff muscles and soothe aching joints, while an ice pack is fantastic for reducing acute inflammation and numbing sharp pain. Many people find that alternating between the two is especially effective.
These aren't just about feeling good in the moment. These therapies can help retrain your body's response to pain signals over time. We see this principle in action across all age groups, which is why our practice also provides focused guidance on issues like managing infant colic and reflux through gentle techniques, showing how targeted, supportive care can make a huge difference.
Key Takeaway: The whole point of assembling a care team is to weave a strong network of support. Your primary doctor, physical therapist, chiropractor, and mental health professional should all feel like partners who are genuinely invested in your well-being.
By fostering open communication and staying curious about a range of therapies, you build a robust system that can catch you when you fall. This collaborative strategy is the foundation for learning how to manage chronic pain effectively, empowering you to move forward with confidence and a sense of control.
Of course. Here is the rewritten section, formatted to sound like an experienced human expert and match the provided examples.
Common Questions About Living with Chronic Pain
Once you start putting these strategies into practice, it’s only natural for new questions to pop up. The day-to-day reality of managing pain can feel different than just reading about it, and that’s completely okay. I hear these same questions from patients all the time as they begin their journey, so think of this as a quick guide to help you stay confident and on track.
How Long Until These Strategies Actually Work?
This is usually the first thing everyone asks, and the most honest answer is: it really depends. Managing chronic pain is a marathon, not a sprint. The goal is to make small, sustainable changes that add up over time, not to find a magic bullet.
You might feel some temporary relief right away from something simple like a heat pack or a few gentle stretches. But the real, foundational work—like adjusting your nutrition, building a consistent movement routine, and shifting your mindset—takes time and consistency to create lasting change. You may notice small improvements in your energy or mood within a few weeks, but significant, durable relief often takes several months of dedicated effort.
It’s so important to be patient and kind to yourself through this. I always tell my patients to keep a simple journal. Tracking your pain levels, energy, and mood can help you see the slow, steady progress that’s easy to miss otherwise.
Is It Safe to Exercise When I'm Already in Pain?
Yes, absolutely—and when done the right way, it’s not just safe, it's essential. The first step is to completely forget the old "no pain, no gain" mentality. That doesn't apply here. For chronic pain, your goal is gentle, restorative movement that sends a signal of safety to your nervous system.
Start slow and keep it low-impact. Think about things like a quiet walk in a park, gentle yoga, or swimming. The most crucial skill to learn is pacing. Doing a little bit every day is far more beneficial than pushing yourself too hard on a good day and triggering a painful flare-up that sets you back.
If any activity causes a sharp spike in your pain or introduces a new kind of pain, that's your body's clear signal to stop and reassess—not to push through it. A physical therapist who specializes in chronic pain can be an incredible resource for creating a plan that is both safe and effective for your specific condition.
How Do I Find a Therapist Who Understands Chronic Pain?
Finding the right mental health professional is a huge piece of the puzzle. You need someone who gets that your pain is real and has specific tools to help you navigate the emotional and psychological weight it carries.
When you're looking, search for a professional who lists "health psychology," "chronic pain," or Cognitive Behavioral Therapy for Pain (CBT-P) in their specialties. Your primary doctor or physical therapist can often give you great referrals to trusted colleagues they work with.
Don't ever feel shy about interviewing potential therapists. On that first call, ask them directly about their experience helping people manage the physical and emotional toll of living with chronic pain. A good fit will focus on practical coping skills and understand the deep connection between mind and body, offering you strategies that go far beyond just talk therapy.
Can I Really Manage Chronic Pain Without Medication?
For many, the answer is a definite yes. A truly holistic approach that combines physical therapy, neurologically-focused chiropractic adjustments, smart nutrition, and lifestyle changes can dramatically reduce—and in some cases, eliminate—the need for daily pain medication.
These strategies work together to address the root causes of pain amplification while boosting your body’s natural ability to heal and self-regulate. They help calm an overactive nervous system, lower inflammation, and restore proper function.
However, medication can still be an important tool for some people, especially for getting through severe flare-ups. The real goal is to work with your entire care team to find the right combination of treatments that improves your quality of life and minimizes side effects. It’s always about what helps you function better and live your life more fully.
At First Steps Chiropractic, we believe in a team approach to health. Our neurologically-focused care is designed to get to the root of your symptoms and help your body heal from the inside out. Whether you’re seeking prenatal support, pediatric care, or relief from chronic pain, our five-step process ensures a personalized plan for your entire family. Schedule your complimentary consultation today!

