When your baby is screaming for hours on end, figuring out why can feel impossible. Is this colic? Is it reflux? Is it something else? You're not alone in this struggle. Both conditions are incredibly common, frequently misunderstood, and their symptoms often overlap, leaving exhausted parents playing a frustrating guessing game.
Let’s clear up the confusion. While both lead to a very unhappy baby, they come from two very different places.
What Is Infant Colic?
At its heart, colic is a behavioral diagnosis. It isn't a disease or an illness, but rather a specific pattern of intense, unexplained crying. The classic definition is the "rule of threes": crying for more than three hours a day, for more than three days a week, for at least three consecutive weeks.
It’s estimated to affect anywhere from 3% to 40% of newborns globally, so if you're in the thick of it, know that countless other parents are too. You can read more about the research behind infantile colic on NCBI.
Key signs of colic usually include:
- Crying that sounds more like intense screaming.
- A predictable fussy period, almost always in the late afternoon or evening (the infamous "witching hour").
- The crying has no obvious trigger—your baby is fed, has a clean diaper, and is otherwise healthy.
- You might see physical signs of distress, like a red, flushed face, tightly clenched fists, or legs pulled up toward their tummy.
What Is Infant Reflux?
Infant reflux, also known as gastroesophageal reflux (GER), is a mechanical issue. It happens when the muscle at the top of the stomach (the lower esophageal sphincter) is still a bit immature and doesn't close tightly. This allows milk and stomach acid to flow back up into the esophagus.
Sometimes this results in simple spit-up, but other times it can cause painful "silent reflux," where the acidic contents come up but are swallowed again instead of being spat out. If you suspect your baby's reflux is painful or isn't always accompanied by spit-up, our guide on the signs and symptoms of silent reflux might offer some clarity.
The biggest clue often lies in the timing. Reflux discomfort is almost always tied to feedings, peaking either during or right after a meal. Colic, on the other hand, can erupt at any time, seemingly out of nowhere.
Here’s a quick breakdown to help you start telling the two apart based on what they fundamentally are.
| Feature | Colic (A Behavioral Pattern) | Reflux (A Mechanical Issue) |
|---|---|---|
| Primary Sign | Intense, inconsolable crying | Spitting up or regurgitation |
| Timing | Often predictable, usually in the evening | Directly related to feeding times |
| Root Cause | Unclear; likely linked to an immature gut or nervous system | Immature lower esophageal sphincter (LES) muscle |
| Main Complaint | Unexplained fussiness | Discomfort from stomach acid |
A Practical Symptom Comparison Guide
When you're in the thick of it with a distressed baby, every cry can start to sound the same. But if you play detective and tune into your baby's specific behaviors, you can uncover some major clues pointing toward either colic or reflux. The trick is to look at the whole picture—not just the crying, but what’s happening before, during, and after each fussy episode.
Getting a handle on the distinct patterns of colic versus reflux is your first real step toward finding something that actually works. While both conditions are tough on everyone, their symptoms are often quite different once you know what you’re looking for. Paying close attention to your baby’s body language, the timing of their fussiness, and how it all relates to feeding can bring a surprising amount of clarity.
Decoding Your Baby's Body Language
A baby’s posture and movements are their main way of telling you they’re in pain. Colic and reflux usually trigger very different physical reactions, and learning to spot them is key.
A baby struggling with colic often looks like a little ball of tension. You’ll probably see:
- Tightly clenched fists and a body that feels rigid or stiff.
- Legs pulled up toward their belly, like they're trying to relieve gas.
- A flushed, red face from the effort of all that intense crying.
On the other hand, a baby dealing with reflux pain tends to make movements that seem aimed at relieving pressure in their chest and throat. This often looks like:
- Arching their back during or right after a feeding, sometimes getting stiff as a board.
- Frequent squirming and restlessness, especially when you lay them down flat.
- Turning their head from side to side, almost as if to get away from the bottle or breast.
This visual decision aid is a great starting point for connecting your baby's crying patterns to a potential cause, whether it's the classic timing of colic or the feed-related signs of reflux.
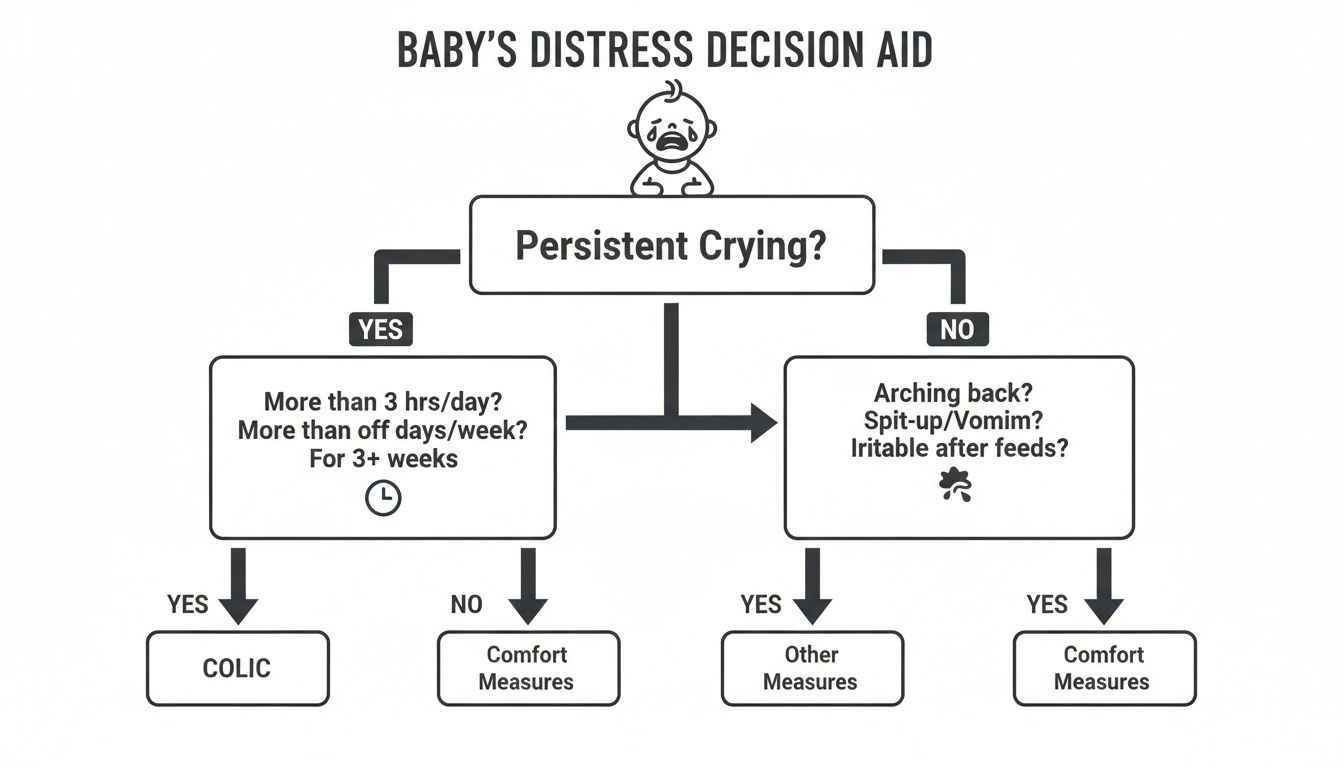
This flowchart helps simplify things by contrasting colic's predictable "witching hour" with reflux's direct link to feeding and spitting up. It guides you toward asking the right questions to figure out what's really going on.
Comparing Symptoms Side-By-Side
To really nail down the difference between colic and reflux, let's look at the most common signs side-by-side. Watching for these patterns over a few days can help you pinpoint the more likely culprit behind your little one’s distress.
A key differentiator is often the context. Colic-related crying frequently seems to appear out of nowhere with no obvious trigger, while reflux-related fussiness is almost always tethered to the act of feeding.
To help you organize your observations, here’s a detailed symptom checker that highlights the subtle but important differences in how your baby might be acting.
Colic vs. Reflux Symptom Checker
| Symptom or Behavior | Common Presentation in Colic | Common Presentation in Reflux |
|---|---|---|
| Timing of Crying | Predictable episodes, often late afternoon or evening ("witching hour"). | Occurs during or immediately after feedings; worsens when lying flat. |
| Body Language | Clenched fists, legs pulled up to the belly, tense abdomen. | Arched back, stiff body, writhing in discomfort. |
| Feeding Patterns | May feed frantically as if trying to soothe, but crying continues. | May refuse to eat, pull away from the breast/bottle, or comfort nurse in short, frequent bursts. |
| Spitting Up | Minimal or unrelated to the crying episodes. | Frequent spitting up or "wet burps"; may be forceful (projectile). Can also be "silent" with no spit-up. |
| Sleep Patterns | Difficulty settling during fussy periods but may sleep well otherwise. | Often wakes up crying in discomfort shortly after being laid down. |
| Sound of Cry | Intense, high-pitched screaming that is difficult to soothe. | Pained, fussy crying that can escalate to screaming, especially after a feed. |
By tracking these specific behaviors, you can build a clearer picture of your baby's experience. This isn't about diagnosing, but about gathering the right information to share with your pediatrician or pediatric chiropractor, so you can find the best path forward together.
Understanding the Root Causes of Infant Discomfort
To truly help your baby find lasting relief, we have to look past the symptoms and ask a simple question: why? Understanding the root cause behind the endless crying or the constant spit-up is the only way to find a real, effective solution. While colic and reflux certainly look different on the surface, you might be surprised to learn how interconnected their root causes can be.
When we break down the difference between colic and reflux, it's easiest to think of one as mainly a mechanical issue and the other as a more complex puzzle with many pieces. But at the end of the day, both are deeply tied to the simple fact that a newborn's tiny body is still figuring things out.
The Mechanics of Infant Reflux
At its core, infant reflux—or gastroesophageal reflux (GER)—is really a plumbing problem. A baby's digestive system is a work in progress, and one of the final parts to get up to speed is the lower esophageal sphincter (LES). This is a small ring of muscle at the top of the stomach that’s supposed to act like a one-way valve.
In many newborns, this little valve just isn't strong or coordinated enough yet. It doesn’t clamp shut as tightly as it should, which allows stomach contents (milk plus stomach acid) to travel back up into the esophagus. This is why spit-up is almost a rite of passage for new babies.
Gastroesophageal reflux (GER) is incredibly common. Some studies show that up to 70% of healthy newborns spit up daily, but this usually resolves on its own by 12-14 months in 95% of cases. For most, this is just a laundry issue, not a medical one. However, when it becomes GERD—causing pain, feeding issues, or poor weight gain—it affects about 12% of infants. You can learn more about the distinctions between GER and GERD in infants.
The Complex Nature of Colic
Unlike the straightforward mechanics of reflux, the true cause of colic is a lot more mysterious. It’s widely considered a multifactorial issue, meaning there isn't one single culprit. Instead, it's likely a perfect storm of contributing factors that lead to those intense, inconsolable crying spells.
Researchers have zeroed in on a few leading theories:
- Gut Immaturity: Just like the LES, a baby’s entire digestive tract is still learning the ropes. This immaturity can lead to painful gas, intestinal spasms, and general discomfort as their gut struggles to process milk efficiently.
- Sensory Overstimulation: A newborn’s nervous system is incredibly sensitive and can get overwhelmed easily. The lights, sounds, and sensations of the world can simply be too much, causing a complete meltdown by the end of the day—what we all know as the "witching hour."
- Developing Microbiome: The community of bacteria in a baby’s gut is just getting established. An imbalance, or dysbiosis, might create inflammation and digestive distress that contributes to colicky behavior.
While these theories point to different triggers, they all share a common thread: an immature, easily dysregulated system is struggling to adapt to life outside the womb. This is where the nervous system steps in as the master regulator of it all.
The Central Role of the Nervous System
Your nervous system is the body's command center, running everything from your heartbeat to your digestion. For the gut, one of the most important players is the vagus nerve. Think of this nerve as a superhighway connecting the brain to the digestive organs, controlling stomach acid, intestinal movement, and even the tightening of the LES valve.
When the nervous system is calm and regulated, digestion runs smoothly. But when it’s under stress, it can send scrambled signals that throw the whole system out of whack. The physical stress from the birth process alone—even in a textbook delivery—can create subtle tension and misalignments in a baby's upper neck and skull.
This physical tension can irritate the vagus nerve and other critical nerves that manage the digestive organs. This irritation, what we chiropractors call subluxation, creates a state of neurological dysregulation.
This dysregulation can show up in two major ways:
- Impaired Digestive Function: Nerve interference can directly mess with the mechanics of digestion. It might weaken the tone of the LES (leading to reflux) or disrupt the rhythmic muscle contractions needed to move milk and gas through the intestines (leading to colic).
- An Overactive "Fight-or-Flight" Response: A stressed nervous system keeps a baby stuck on high alert. This makes them extra sensitive to their environment, much harder to soothe, and more likely to have those inconsolable crying jags that are the hallmark of colic.
This neurological link explains why two very different issues—colic versus reflux—often show up together or have overlapping symptoms. Both can be traced back to underlying nervous system stress that’s keeping the body from working the way it should, which paves the way for holistic solutions that get to the root of the problem.
Effective Soothing Strategies and Management Techniques

When you're in the thick of it with a relentlessly crying baby, you need a solid toolkit of soothing strategies. The goal isn't just to quiet the cries for a moment, but to bring genuine comfort by addressing what's causing their distress in the first place. These techniques can be as simple as changing the way you hold your baby or as specific as specialized care, all with the shared mission of bringing peace back into your home.
It's important to remember that this is often a process of trial and error. What works wonders for one baby might do nothing for another. The real key is patience—staying observant and learning to read the subtle cues your little one is sending you.
At-Home Comfort and Positional Care
Sometimes the most profound changes come from the simplest adjustments in your daily routine, especially for babies dealing with reflux. Gravity can be your greatest ally here. By holding your baby upright for 20-30 minutes after they eat, you can help keep their milk and stomach acid right where they belong.
This one simple step prevents the easy backflow that causes so much discomfort. You can hold them over your shoulder, sit them up on your lap, or even use a baby carrier to keep your hands free. For many families, this single change dramatically cuts down on post-feeding fussiness.
Mastering the art of burping is another cornerstone of at-home care. Babies with colic often gulp down a lot of air during those intense crying fits, while trapped gas can make reflux pain much worse.
- Over-the-Shoulder: The classic position, gently patting or rubbing their back.
- Sitting Up: Support your baby’s chest and head with one hand as they sit on your lap, leaning them forward just a bit.
- Tummy-Down: Lay your baby belly-down across your lap, making sure their head is slightly higher than their chest.
A common mistake is to give up on burping too quickly. Try to spend a few dedicated minutes on it after every single feeding, even if you don't get an immediate result. That one delayed burp can be the difference between a peaceful nap and another round of crying.
Creating a calm, low-stimulation environment is also a game-changer. This is particularly true for a colicky baby whose nervous system can be easily overwhelmed. Dim the lights, turn on a white noise machine to mimic the gentle sounds of the womb, and swaddle them snugly for a feeling of security. These steps help dial down their "fight-or-flight" response and encourage relaxation.
Conventional Medical and Dietary Approaches
If at-home strategies aren't providing enough relief, it's time to talk to your pediatrician about conventional treatments. These typically start with dietary changes and, for more severe reflux, may include medication.
For moms who are breastfeeding, what you eat can sometimes affect your baby. Common triggers that can pass through breast milk include dairy, soy, eggs, and caffeine. Working with your doctor to try an elimination diet can help you pinpoint if something in your diet is contributing to the problem.
If you're formula-feeding, your pediatrician might suggest trying a different kind of formula. The main options are:
- Hypoallergenic Formulas: These are made with proteins that are already broken down, making them much easier for a sensitive tummy to digest.
- Thickened Formulas: Some formulas have added rice starch to make them heavier, which helps the milk stay in the stomach and reduces spit-up.
For clear cases of gastroesophageal reflux disease (GERD), where a baby is in obvious pain or not gaining weight properly, medication may be necessary. Acid-suppressing drugs, like H2 blockers or proton pump inhibitors (PPIs), can be prescribed to make stomach contents less acidic and spit-up less painful. This is not a first-line treatment for simple reflux, however, and is usually reserved for cases with a clear medical need due to potential side effects.
Neurologically-Focused Chiropractic Care
More and more parents are looking for solutions that get to the root cause of their baby's discomfort, not just mask the symptoms. This is where neurologically-focused pediatric chiropractic care comes in, offering a gentle and unique perspective. This is not about "cracking" a baby's spine; it involves incredibly light, specific touches.
The guiding principle is that the physical stress of the birth process can create tiny misalignments in the spine, especially in the upper neck. These misalignments, called subluxations, can interfere with the nervous system—the body's master control system.
The vagus nerve, a major player in regulating both digestion and the body's calming response, exits the brainstem right at the top of the neck. When there's physical tension in this area, it can disrupt the signals this vital nerve sends to the gut. This interference can show up as poor digestion (reflux, gas) and a nervous system stuck in a high-stress state (colicky crying).
A pediatric chiropractor uses gentle, precise adjustments—often with no more pressure than you'd use to check a tomato for ripeness—to relieve this tension. By restoring proper alignment and movement, the goal is twofold:
- Improve Nerve Communication: Releasing pressure on the nerves that control the digestive system can lead to better gut motility, less gas, and a more effective lower esophageal sphincter (LES).
- Calm the Stress Response: Easing this physical tension helps shift the baby’s nervous system out of a constant "fight-or-flight" mode and into a more relaxed "rest-and-digest" state.
This approach is all about helping the body heal and regulate itself from the inside out. By addressing the underlying neurological dysregulation, many parents report profound relief from both colic and reflux. You can learn more about this process in our guide to finding colic relief for newborns. It's a non-invasive path that can lead to a calmer baby and a much more peaceful household.
When You Should Seek Professional Help
Parental intuition is a powerful thing. While most cases of colic and reflux are more exhausting than dangerous, you know your baby best. If something feels off, trust that gut feeling. It’s crucial to know the difference between typical baby fussiness and a genuine medical issue, and recognizing the red flags can help you act quickly when it matters most.
It's also important to remember where different types of care fit in. Supportive approaches, like positioning changes or gentle chiropractic adjustments, are designed to work alongside your pediatrician's medical oversight, not replace it. These methods can bring incredible comfort and help with underlying functional issues, but they don't take the place of a medical evaluation when serious symptoms pop up.

Recognizing Red Flag Symptoms
Some signs just aren't normal and signal that it's time for immediate professional help. These symptoms point to something more serious than uncomplicated colic or reflux and need to be checked out by a medical doctor right away. Don’t wait to call your pediatrician or head to urgent care if you see any of the following.
- Projectile Vomiting: This is more than just a big spit-up. We're talking forceful vomiting that can shoot several feet across a room. This can indicate a physical blockage.
- Poor Weight Gain or Weight Loss: Your baby should be steadily packing on the ounces. If they’re struggling to gain weight or, worse, losing it, it’s a clear sign they aren't keeping enough nutrition down.
- Blood in Spit-Up or Stool: Any sign of blood, whether it's bright red streaks or dark flecks that look like coffee grounds, needs to be evaluated immediately.
- Breathing Difficulties: This includes any wheezing, a chronic cough, gasping, or scary pauses in breathing (apnea). Any respiratory issue is a reason to seek immediate medical attention.
Your job is to be your baby's advocate. Don't be afraid to document what you're seeing. Taking a quick video or photo on your phone can be incredibly useful when you talk to the doctor, giving them a clear picture of what’s happening at home.
When to Make the Call
Beyond those urgent red flags, other signs suggest your baby's discomfort is getting worse and warrants a doctor's visit.
Significant Lethargy or Change in Demeanor
If your baby is suddenly unusually sleepy, hard to wake for feedings, or seems floppy and limp, they need to be seen right away. A drastic shift in their energy or responsiveness is a major warning sign.
Signs of Dehydration
Dehydration can happen fast in a little one. Keep an eye out for fewer wet diapers (less than six in 24 hours), a sunken soft spot on their head, crying with no tears, and a dry mouth.
High Fever
For any baby under three months old, a rectal temperature of 100.4°F (38°C) or higher is a medical emergency. Don't second-guess it—call your doctor or go to the emergency room.
While exploring options like neurologically-focused care can be a fantastic way to get to the root of your baby’s discomfort, the first step is always to rule out any underlying medical problems with your pediatrician. An integrated approach ensures your baby is safe and supported from all angles. To learn more about how a healthy nervous system plays a role, check out our overview of chiropractic care for babies.
Your Questions About Colic and Reflux, Answered
Navigating the world of infant discomfort can feel like wading through a sea of uncertainty. When your baby is in distress and you're searching for answers, having clear, straightforward information is everything. This section tackles the most common questions that pop up when parents are trying to figure out if they’re dealing with colic, reflux, or something else entirely.
Every baby’s story is unique, but the core concerns you’re facing are shared by so many parents. Getting a handle on these key points can make a world of difference in how you approach your baby’s care with confidence.
Can My Baby Have Both Colic and Reflux?
Yes, and it’s actually quite common for a baby to have both conditions at the same time, which is what makes getting a clear diagnosis so tricky. The symptoms overlap so much that they can create a really confusing picture for parents.
Think of it this way: the constant pain and discomfort from reflux can easily trigger the intense, inconsolable crying episodes that define colic. In that scenario, reflux is the root problem, and the colic-like crying is a symptom of that underlying issue. This is exactly why a thorough, comprehensive evaluation is so crucial.
A skilled provider can help you sort out whether one condition is causing the other or if both are present on their own. By getting to the root cause—like nervous system irritation that can mess with both gut function and stress levels—you can often bring relief to symptoms of both conditions.
How Does Pediatric Chiropractic Care Help These Conditions?
Pediatric chiropractic care zeros in on the powerful connection between the spine and the central nervous system. The physical stress of birth, even in a smooth delivery, can cause tiny misalignments in the spine. This is especially true in the upper neck, where some really critical nerves are located.
These subtle shifts can interfere with how key nerves function, especially those that control digestion and relaxation—most notably, the vagus nerve. When the vagus nerve gets irritated, it can disrupt the signals going to the digestive tract, which can contribute to reflux, gas, and those painful intestinal spasms.
Gentle, specific adjustments are designed to restore proper nerve communication. The goal is to improve digestive function, reduce physical tension throughout the baby's body, and calm their overactive stress response. This approach addresses a potential root cause of discomfort, leading to a happier, more settled infant.
The pressure used is incredibly light—often no more than you’d use to check if a peach is ripe. It’s a non-invasive way to help the body regulate itself and work the way it was designed to.
What Can I Do for Immediate Soothing Tonight?
When you’re in the middle of a tough evening, having some immediate, go-to soothing techniques can be a lifesaver. For quick comfort, many parents find huge success with the "Five S's" method, which helps recreate the calming sensations of the womb.
These five steps are:
- Swaddling: Wrapping your baby up snugly helps them feel secure and prevents their startle reflex from waking them.
- Side/Stomach Position: Holding your baby on their side or stomach can be very calming (just remember, this is only while they are awake and you are holding them).
- Shushing: Making a loud, consistent "shushing" sound mimics the noise inside the womb and can be incredibly soothing.
- Swinging: Gentle, rhythmic motion like rocking or swaying is deeply calming for a distressed baby.
- Sucking: Offering a pacifier or even a clean finger engages their natural calming reflex.
If you have a hunch that reflux is part of the problem, remember to keep your baby upright for at least 20-30 minutes after every single feeding. Gentle tummy massages and "bicycle leg" motions can also do wonders for relieving the gas pressure that often rides along with both conditions.
Will My Baby Eventually Outgrow These Issues?
The short answer is yes, most babies do. Colic usually hits its peak around six weeks and then resolves on its own by three to four months as the baby's nervous system matures. Likewise, simple reflux typically gets much better by 12 months as their digestive system gets stronger and they start spending more time upright.
But just "waiting it out" can be incredibly stressful and exhausting for the entire family. If there's an underlying neurological or structural issue contributing to the discomfort, symptoms might stick around longer or even morph into other challenges down the road.
Getting to the root cause with supportive care can shorten how long and intense these challenges are. This not only brings relief in the short term but also helps promote healthier overall development for a more comfortable and connected start to life.
At First Steps Chiropractic, we specialize in gentle, neurologically-focused care to help your baby's system find balance and calm. If you're struggling to understand the difference between colic versus reflux, a complimentary consultation can help provide the clarity and support you need. Learn more about our approach at https://firststepschiropractic.com.

