If you’ve found your way here, chances are you’re noticing some things about your child that are hard to put into words. Maybe they’re intensely bothered by the seams in their socks, get completely overwhelmed by the noise in a busy store, or seem to be in constant, restless motion.
You are not alone on this journey, and there are very real, neurological reasons behind these behaviors. This guide is designed to be your roadmap, helping you make sense of it all.
Our goal here is to pull back the curtain on Sensory Processing Disorder (SPD) and Auditory Processing Disorder (APD). We’ll break down these complex topics into clear, understandable pieces.
Think of your child’s brain and nervous system as a busy city’s traffic control center. In a typically developing child, a skilled air traffic controller directs all the incoming information smoothly. Cars, buses, and bikes (all the sensory inputs) move to their destinations without a hitch.
When the Traffic Controller Gets Overwhelmed
Now, for a child with a sensory and auditory processing disorder, that internal traffic controller is struggling to keep up. The signals get tangled, sent down the wrong roads, or misinterpreted entirely. It’s a neurological traffic jam.
- Sensory Processing Disorder (SPD): This is like a city-wide gridlock. The brain’s control center has trouble managing all kinds of sensory information—touch, sight, sound, taste, smell, and even internal signals like balance and body awareness.
- Auditory Processing Disorder (APD): This is more like a problem with the radio dispatch system. The ears are working perfectly and hearing all the sounds, but the control center can't make sense of the messages coming through, especially when there’s a lot of background chatter.
This neurological "traffic jam" can show up very early on. Understanding how to spot sensory issues in infants can give you incredible insight into how these challenges take root from the very beginning. It's crucial to know this isn't a behavioral choice; it's a fundamental difference in how their brain is wired.
A child's reaction to the world is not defiance—it's a direct reflection of their nervous system's capacity to process everything coming at them. Grasping this simple fact is the first, most powerful step toward providing the right kind of support.
Throughout this guide, we'll walk you through everything you need to know, step-by-step. We will explore the common signs of SPD and APD at different ages, unpack the key differences between them, and look at the neurobiology behind it all. Most importantly, we'll map out the proven pathways for getting a clear diagnosis and the effective interventions that can help your child’s nervous system finally find calm and regulation.
Decoding Sensory vs. Auditory Processing Disorder
When you're navigating the world of your child's health and development, it can feel like you're learning a whole new language. You might hear terms like Sensory Processing Disorder (SPD) and Auditory Processing Disorder (APD), and it's easy to get them confused. They can sound similar and even overlap, but they actually describe very different challenges for your child.
Getting clear on the difference is one of the most important first steps you can take to find the right path forward.
The Broad Highway vs. The Specific Radio Frequency
Let's break it down with an analogy. Think of your child’s brain and nervous system as a complex highway network, constantly managing traffic from all over the body.
-
Sensory Processing Disorder (SPD) is like a massive, system-wide traffic jam. Information coming from every on-ramp—the eyes (sight), skin (touch), ears (sound), muscles (proprioception), and inner ear (balance)—is getting stuck, misdirected, or even crashing. This creates chaos across the entire network, impacting how your child moves, feels, and reacts to the world around them. It’s a challenge with the entire operating system for the senses.
-
Auditory Processing Disorder (APD), on the other hand, is like a problem on one specific radio frequency. The traffic on the highway is flowing just fine, but the brain’s radio receiver can’t quite tune into the traffic reports. The sound comes through, but it’s garbled, distorted, or lost in background static. The child’s ears are working perfectly, but the brain struggles to make sense of what it’s hearing.
This simple diagram shows the three core stages of how the brain handles any sensory signal: input, processing, and then the behavioral output we see.
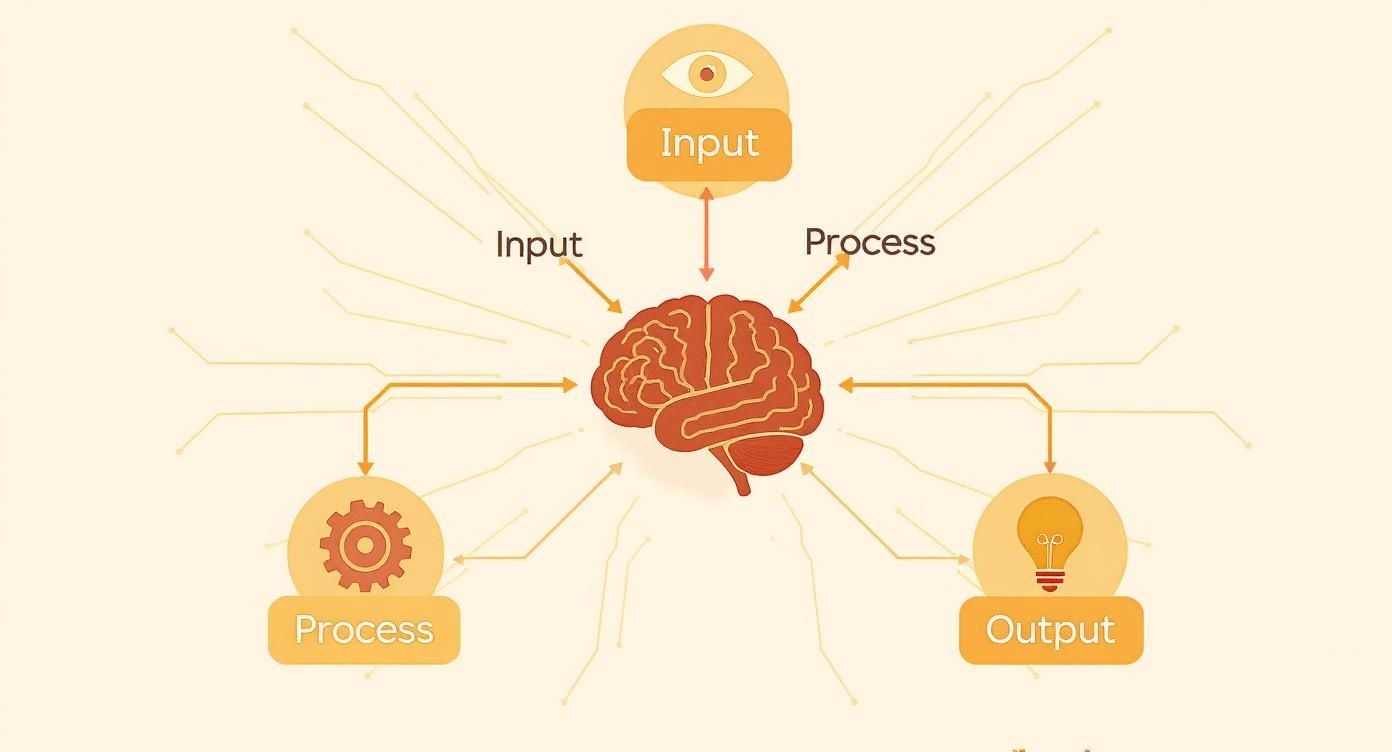
Both SPD and APD originate in that middle “Process” stage. A breakdown there is what ultimately leads to the "Output," or the behaviors and challenges we notice in our kids.
SPD vs. APD At a Glance
While both disorders are rooted in how the brain processes information, they show up very differently in a child's day-to-day life. Here’s a table to help clarify the key distinctions.
| Feature | Sensory Processing Disorder (SPD) | Auditory Processing Disorder (APD) |
|---|---|---|
| Primary Area Affected | Affects how the brain handles information from any of the eight senses (touch, sound, sight, movement, etc.). | Specifically affects the brain's ability to interpret and make sense of what the ears hear. |
| Core Challenge | The brain struggles to integrate and respond appropriately to all kinds of sensory input coming in at once. | The brain struggles to distinguish, remember, or sequence auditory information, especially with background noise. |
| Common Signs | Extreme reactions to textures, lights, or sounds; unusual clumsiness; constant need for movement or crashing. | Difficulty following spoken directions, frequently asking "what?", easily distracted by noise. |
| Typical Evaluator | Occupational Therapist (OT) with specialized training in sensory integration. | Audiologist through a series of specialized listening tests in a sound-treated booth. |
Understanding these differences is key, because it’s not just a matter of semantics—it determines who you see for help and what kind of support your child receives.
It's also crucial for parents to know that these conditions are not as rare as you might think. Research suggests that 5% to 16.5% of the general population experiences symptoms of sensory processing challenges. Some studies even estimate it could affect as many as 20% of people. You can find more data on sensory processing disorder prevalence on Frontiers.
Here’s the key takeaway: A child with SPD might have auditory sensitivities, like finding a vacuum cleaner unbearable. That's because sound is just one of the many senses their brain is struggling to regulate. But a child with APD has a specific breakdown in understanding that sound, even if the volume doesn't bother them. This distinction is vital for getting the targeted, effective support your child truly needs.
Recognizing the Signs of SPD and APD in Your Child
Knowing what to look for is the first and most powerful step toward understanding your child's world. The signs of a sensory and auditory processing disorder aren't always obvious—in fact, they often show up looking like behavioral quirks or even defiance. But these behaviors are your child's way of communicating that their nervous system is struggling to manage the world around them.
The signs can also change dramatically as a child grows. What you see in a baby will look completely different from the challenges a school-aged child faces, which is why it helps to look at them through the lens of different developmental stages.

Signs in Infants and Toddlers (Ages 0-3)
In these earliest years, the signs are often tied to core functions like feeding, sleeping, and just being comfortable. An infant’s nervous system is just beginning to organize itself, and any struggles with sensory processing can create significant distress for them (and you).
- Extreme Fussiness: The baby seems unusually difficult to soothe and may cry inconsolably for long stretches.
- Feeding Difficulties: They might struggle with latching, refuse certain bottle nipples, or have intense, negative reactions to the texture of new foods.
- Sleep Challenges: The infant has a hard time settling down for sleep or wakes frequently, seemingly without reason.
- Aversion to Touch: They may arch their back or cry when held, cuddled, or swaddled, avoiding the very comfort you're trying to provide.
- Delayed Milestones: Milestones like rolling over, sitting up, or crawling might be delayed because of challenges with motor coordination and body awareness.
When it comes to APD, an early sign can be a noticeable delay in speech and language. You might also notice the child doesn't turn their head toward sounds as expected. Or, they might have one of two extreme reactions: being intensely startled by everyday noises or seeming to ignore them completely.
Signs in Preschoolers (Ages 3-5)
As a child's world expands to include preschool and more social time, the signs of SPD and APD can become much more apparent in how they play and interact with others. This is often the age where parents really start to notice their child is responding differently than their peers.
During this stage, you might see clear examples of the three main types of sensory responses:
- Over-Responsivity (Sensory Defensiveness): The child has an exaggerated reaction to sensory input. Think of the kid who covers their ears at the sound of a blender, refuses to wear clothes with tags, or avoids messy play with paint or sand at all costs.
- Under-Responsivity: This child seems to have a muted response to sensations. They might not notice when their hands or face are dirty, have an unusually high tolerance for pain, or appear lethargic and slow to respond.
- Sensory Seeking: This child has an intense craving for sensory input. They are in constant motion—crashing into furniture, spinning in circles, and seeking out loud noises and bright lights.
For APD, preschoolers may struggle to follow simple, one-step directions. In a noisy classroom, they can seem "tuned out" or lost, simply unable to filter their teacher's voice from all the background chatter.
A key observation for parents is recognizing that these behaviors aren't choices. A child who constantly fidgets isn't trying to be disruptive; their body is trying to get the input it desperately needs to feel organized and focused.
Signs in School-Aged Children (Ages 6+)
Once a child enters elementary school, the academic and social demands ramp up significantly. This new environment can magnify underlying sensory and auditory processing challenges, making them much more visible in the structured classroom setting.
Common signs of sensory processing disorder in this age group include:
- Difficulty with Focus: The child is easily distracted by sights or sounds in the classroom, constantly fidgets in their chair, or chews on their shirt collar.
- Poor Motor Skills: They might have messy handwriting, appear clumsy on the playground, or struggle with tasks requiring fine motor control, like tying their shoes.
- Social and Emotional Challenges: The child may have trouble with personal space (standing too close or too far away), get easily overwhelmed in groups, or have intense emotional outbursts that seem way out of proportion to the situation.
For a child with auditory processing disorder, school can feel like an uphill battle every single day. Their struggles might look like this:
- Trouble with Multi-Step Directions: They can follow the first step but get completely lost on the second or third.
- Frequent Misunderstandings: They often mishear words (like hearing "boat" instead of "coat") and may constantly ask "What?" or "Huh?"
- Academic Struggles: Reading, spelling, and following lectures can be incredibly difficult because their brain is working overtime just to decode the sounds everyone else hears effortlessly.
Recognizing these patterns is that crucial first step. If these signs resonate with you, it’s not a cause for alarm. Instead, see it as a call to action—an invitation to dig deeper and find the support that can help your child’s nervous system finally thrive.
Exploring the Neurological Roots of Sensory Challenges
When your child struggles with sensory input, it's easy to see it as a behavioral problem. But after decades of research, we know these challenges aren't a choice. They're rooted deep in the brain's structure and how it functions. Shifting our perspective is the first, most crucial step in getting our kids the right support.
Think of your child’s brain as a bustling city full of super-highways. These highways are made of white matter, which is like the brain's communication wiring, zipping information from one place to another. For a child dealing with a sensory or auditory processing disorder, it’s like some of these critical highways have constant construction, detours, or confusing traffic patterns.
Brain-Based Evidence for Sensory Differences
For too long, parents were told these issues were "all in their child's head," but now we have solid proof that SPD is a brain-based condition. A groundbreaking 2013 study from UC San Francisco used advanced imaging to get a direct look at these neural highways.
The researchers found clear evidence that children with SPD have measurable, structural differences in their white matter tracts. These differences were most significant in the back part of the brain, which is responsible for sorting through sensory data. The study showed a direct link between these brain differences and the sensory struggles a child experiences, with the strongest connection found for auditory processing.
This research was a huge moment—it validated what parents knew all along. Their child's experience is real, and it has a biological cause.
The Brain’s Sensory Management Team
Three key parts of the brain have to work together perfectly as a "sensory management team." When this team isn't in sync, sensory signals get disorganized and jumbled.
- Brainstem: This is the first stop for all incoming sensory information, like a busy mail sorting room. It makes the initial call on what's important enough to pass along and what’s just background noise.
- Thalamus: Think of the thalamus as the brain’s main switchboard operator. It takes the sorted signals and directs them to the right "departments" for processing.
- Cerebral Cortex: This is the executive office where we make sense of it all. The cortex is where raw data is turned into a recognizable sound, a clear image, or a distinct feeling.
For a child with SPD or APD, this intricate relay system can have glitches at any point, leading to a confusing and disorganized response. This is a fundamental concept in understanding how the nervous system works and its central role in everything we perceive and do.
The Hopeful Power of Neuroplasticity
Now for the best part of the story: the brain isn't static. It has an incredible, lifelong ability to change, adapt, and build new connections. This is a concept called neuroplasticity. Just like a muscle gets stronger with exercise, the brain can build stronger, more efficient neural pathways with the right kind of targeted input.
This means that your child’s challenges are not a life sentence. They represent a neurological difference that can be supported, strengthened, and rewired over time. Targeted therapies and interventions don't just teach coping skills; they physically change the brain for the better.
This understanding shifts us from seeing a child's struggles as a behavioral issue to viewing them as a neurological opportunity. By providing specific, focused support, we can help their brain forge those new, more effective "super-highways," allowing them to navigate their world with more confidence, calm, and regulation.
How to Navigate Diagnosis and Build Your Support Team
Once you start seeing the signs and get that gut feeling that your child might be struggling with a sensory or auditory processing disorder, the next question is a big one: what do we do now? The path to getting clear answers can feel overwhelming, but it’s a journey you don’t have to take alone. It all starts with building a dedicated team of professionals who can provide a clear diagnosis and guide you toward effective, evidence-based support.
Think of it like renovating a house. You wouldn't hire a plumber to do the electrical work; each professional has a distinct and vital role. The same is true for your child's care team.
Creating a collaborative team is the single most powerful step you can take. When these pros communicate with each other and with you, everyone gets a complete picture of your child's needs and can work from a unified plan to help them thrive.
Who to See for an Evaluation
Your journey will likely kick off with your pediatrician, who can offer referrals and rule out any other medical issues. From there, three key specialists are central to diagnosing and supporting sensory and auditory challenges. Each one brings a unique and critical lens to understanding your child.
-
The Audiologist for APD: An audiologist is the only professional who can formally diagnose Auditory Processing Disorder. They use a series of specialized tests in a sound-treated booth to see how the brain is interpreting what the ears are hearing. This goes way beyond a standard hearing test—it’s an evaluation of the central auditory nervous system’s performance.
-
The Occupational Therapist for SPD: An Occupational Therapist (OT), especially one with advanced training in sensory integration, is your go-to expert for a Sensory Processing Disorder evaluation. They use a mix of standardized assessments, clinical observations of your child at play, and detailed parent questionnaires to identify specific patterns of sensory over-responsivity, under-responsivity, or seeking.
-
The Speech-Language Pathologist for Communication: A Speech-Language Pathologist (SLP) becomes essential when auditory processing issues start to impact communication. They assess how a child understands and uses language, follows directions, and hangs in a conversation, especially when there’s background noise. An SLP often works hand-in-hand with the audiologist to address the real-world impact of APD.
What to Expect During Assessments
The evaluation process isn't just a checklist; it's a deep dive into your child's unique neurological profile. It involves carefully observing how your child moves, plays, listens, and responds to various sensory inputs in a controlled setting.
Assessments usually include a mix of standardized tests (which compare your child's performance to their peers) and structured clinical observations. The therapist will be watching how your child reacts to different textures, movements, and sounds. This combination of data gives the professional a rich, detailed understanding of how their nervous system works.
The goal of an evaluation is not just to get a label. It's to create a detailed roadmap that highlights your child’s specific strengths and pinpoints the exact areas where their nervous system needs more support.
Evidence-Based Interventions That Work
Once you have a clear picture, your team will recommend interventions designed to help rewire the brain’s neural pathways through what's known as neuroplasticity. The entire focus is on building stronger, more efficient connections for processing sensory information.
Key therapies include:
- Occupational Therapy with a Sensory Integration (SI) Approach: This is the gold standard for SPD. In a sensory gym, an OT uses swings, trampolines, and other specialized equipment to give the child targeted sensory input in a fun, play-based way. The goal is to help the child's nervous system get better at organizing and responding to sensations.
- Auditory Therapy: For APD, an audiologist or SLP might recommend specific listening programs. These often involve using headphones to listen to specially modified music or sounds that train the brain to better process auditory information.
- Speech Therapy: An SLP will work on the skills directly hit by APD, like improving the ability to tell the difference between similar-sounding words, follow complex directions, and boost listening comprehension when there's background noise.
Building this team is a proactive, hopeful step toward helping your child feel more calm, confident, and regulated in their world.
Practical At-Home Strategies to Support Your Child
Creating a supportive and predictable home environment is one of the most powerful things you can do to help your child’s nervous system feel safe and regulated. While professional therapies are absolutely essential, the strategies you build into your daily life can make a huge difference in reducing overwhelm and building resilience.
These at-home adjustments aren't a list of strict rules. Instead, think of them as a way of fine-tuning your child's world to better match their unique neurological needs.

Introducing the Sensory Diet
One of the most effective tools OTs recommend is a sensory diet. Now, this has nothing to do with food. It’s a personalized plan of activities designed to give your child the exact sensory input their body needs to stay focused and organized throughout the day. A well-designed sensory diet helps prevent sensory meltdowns before they even start.
Every sensory diet is tailored to a child’s specific profile—whether they're sensory seeking, over-responsive, or under-responsive. The key is to weave these activities into their daily routine for consistent, regulating input.
Examples of sensory diet activities might include:
- Calming Activities: Gentle swinging in a hammock offers great vestibular input, while the deep pressure from a weighted blanket can be incredibly soothing and organizing for the nervous system.
- Alerting Activities: Bouncing on a mini-trampoline or doing "animal walks" (like crab walks or bear crawls) provides powerful proprioceptive input that can wake up a sluggish nervous system.
- Focusing Activities: Squeezing therapy putty or playing with kinetic sand gives just the right amount of tactile input to help a child concentrate on tasks like homework or listening to a story.
For a deeper dive into the professional approaches that complement these strategies, you can learn more about different types of sensory processing disorder therapy and how they are structured.
Modifying Your Environment for Success
Beyond scheduled activities, simple changes to your home can make a world of difference for a child with a sensory and auditory processing disorder. The main goal is to reduce the unpredictable or overwhelming sensory stimuli that can trigger stress and dysregulation. This creates a safe base where their nervous system can finally rest and recharge.
A great place to start is by creating a designated "calm-down corner" like the one pictured above. This isn't a timeout spot; it's a safe haven your child can choose to go to when they feel overwhelmed. Stock it with soft pillows, a weighted lap pad, calming fidget toys, and noise-canceling headphones.
Key Insight: A predictable environment creates a neurologically safe space. When a child’s brain doesn’t have to work so hard to process a chaotic environment, it has more resources available for learning, connecting, and regulating emotions.
Here are a few more high-impact changes you can make:
- Minimize Visual Clutter: Use storage bins to organize toys and try to keep surfaces clear. A visually simple space is far less demanding on the brain.
- Soften the Soundscape: Lay down rugs and hang curtains to absorb excess noise. Keep noise-canceling headphones handy for loud tasks like vacuuming or for trips to busy public places.
- Establish Predictable Routines: A visual schedule showing the day's flow helps your child know exactly what to expect. This simple tool can drastically reduce anxiety and meltdowns related to transitions.
Implementing these strategies empowers your child, helping them feel more in control and better equipped to navigate the challenges of their day.
Answering Common Questions from Parents
As a parent navigating the world of a sensory and auditory processing disorder, you’re going to have questions. This journey is often filled with confusing moments, deep concerns, and a real need for clear, straightforward answers. We’ve put together this Q&A to tackle some of the most common and pressing questions we hear from parents just like you.
Can My Child Outgrow Sensory or Auditory Processing Disorder?
This is one of the first things parents ask, and it comes straight from the heart. While children don't technically "outgrow" the underlying neurological wiring that causes SPD or APD, they can absolutely learn powerful ways to manage it. The challenges don't have to define their lives.
Think of it like this: the brain's ability to create new connections, a process called neuroplasticity, is your greatest ally here. Through targeted therapies like OT and speech therapy, we help the brain build new, more efficient pathways for making sense of the world. The goal isn't a "cure" in the traditional sense; it's to shrink the disorder's impact on their learning, friendships, and happiness. Many kids and teens learn to handle their sensory needs so well that the issues become far less noticeable over time. It’s a journey of adaptation, not just waiting for them to grow out of it.
The real focus is on empowering your child with the tools they need to thrive. With the right support, they learn to navigate their world with confidence, turning what feel like huge obstacles into manageable parts of their day.
Is This the Same Thing as Autism?
This is a fantastic and really important question because there’s so much overlap in the signs. While sensory processing challenges are a core feature of Autism Spectrum Disorder (ASD)—in fact, research shows up to 96% of autistic individuals have them—a child can absolutely have SPD or APD all on its own.
The main difference is that an ASD diagnosis also includes persistent struggles with social communication and interaction, plus restricted or repetitive patterns of behavior.
Here’s a simple way to look at it:
- Most people with autism have significant sensory issues.
- But not everyone with sensory issues has autism.
This is why a comprehensive evaluation from a multidisciplinary team is so critical. It’s the only way to get a clear picture and make sure your child gets the right support plan for their specific needs.
How Do I Explain My Child's Needs to Their School?
Being your child’s advocate at school is one of the most powerful things you can do for them. The key is open, proactive communication to build a real partnership with their teachers.
Start by requesting a meeting with their teacher, the principal, and the school psychologist. It helps to walk in prepared. Bring a simple, one-page summary from your child’s occupational therapist or doctor that explains their specific challenges and, more importantly, lists practical, recommended accommodations.
Instead of just presenting a list of problems, frame it as a collaborative effort to find solutions. For example:
- "To help him focus during lessons, a wiggle cushion at his desk or a few scheduled movement breaks would make a world of difference."
- "We’ve found that preferential seating away from noisy spots like the door or pencil sharpener really helps him stay regulated."
- "Allowing noise-reducing headphones during loud events like assemblies can prevent a complete sensory overload."
Sometimes, the simplest accommodations—like providing written instructions along with verbal ones or giving a little extra time to switch between activities—can completely transform your child’s entire school day for the better. When you approach it as a team, you empower the school staff to become your strongest allies. Your expertise as a parent, combined with their knowledge as educators, creates the perfect partnership for your child’s success.
At First Steps Chiropractic, we understand the intricate connection between the nervous system and your child’s ability to process their world. Our neurologically-focused approach is designed to get to the root cause of these challenges, helping their system find balance and regulation. If you’re ready to explore a different path and get clear answers, schedule your complimentary consultation today. Discover how a well-regulated nervous system can unlock your child's full potential by visiting us at https://firststepschiropractic.com.

