Yes, there is an incredibly strong link between ADHD and what most people would call significant mood swings.
Even though it's not listed as an official symptom for diagnosis, intense emotional shifts are a core, and often misunderstood, part of the ADHD experience for so many people. This emotional rollercoaster isn't a choice or a lack of self-control; it comes down to real differences in the brain's wiring and how it functions.
The Real Link Between ADHD and Mood Swings
If you have ADHD, you might feel like your emotions are hooked up to a hair-trigger. A small, everyday frustration can suddenly feel like a world-ending catastrophe, sparking a flash of anger or a wave of despair that disappears almost as quickly as it arrived.
This experience has a name: emotional dysregulation. Think of it like having an emotional volume dial that’s broken—it jumps straight from a quiet ‘one’ to a blaring ‘ten’ with no stops in between.
Simply understanding this connection can be a huge relief. It’s a powerful first step to realize that these overwhelming feelings have a neurological reason. This isn't some flaw in your character; it's just how your brain is built to process the world. If you want to dive deeper, you can explore our detailed guide on what is ADHD.
And this isn't just a feeling; research backs it up. One study found that over 50% of adults with ADHD struggle with significant emotional swings. For comparison, only 5% of adults without ADHD reported the same thing, which really shows how common this challenge is. You can read the full research about ADHD and emotional instability here.
This infographic does a great job of showing the difference between how things might look on the outside versus what’s happening on the inside.
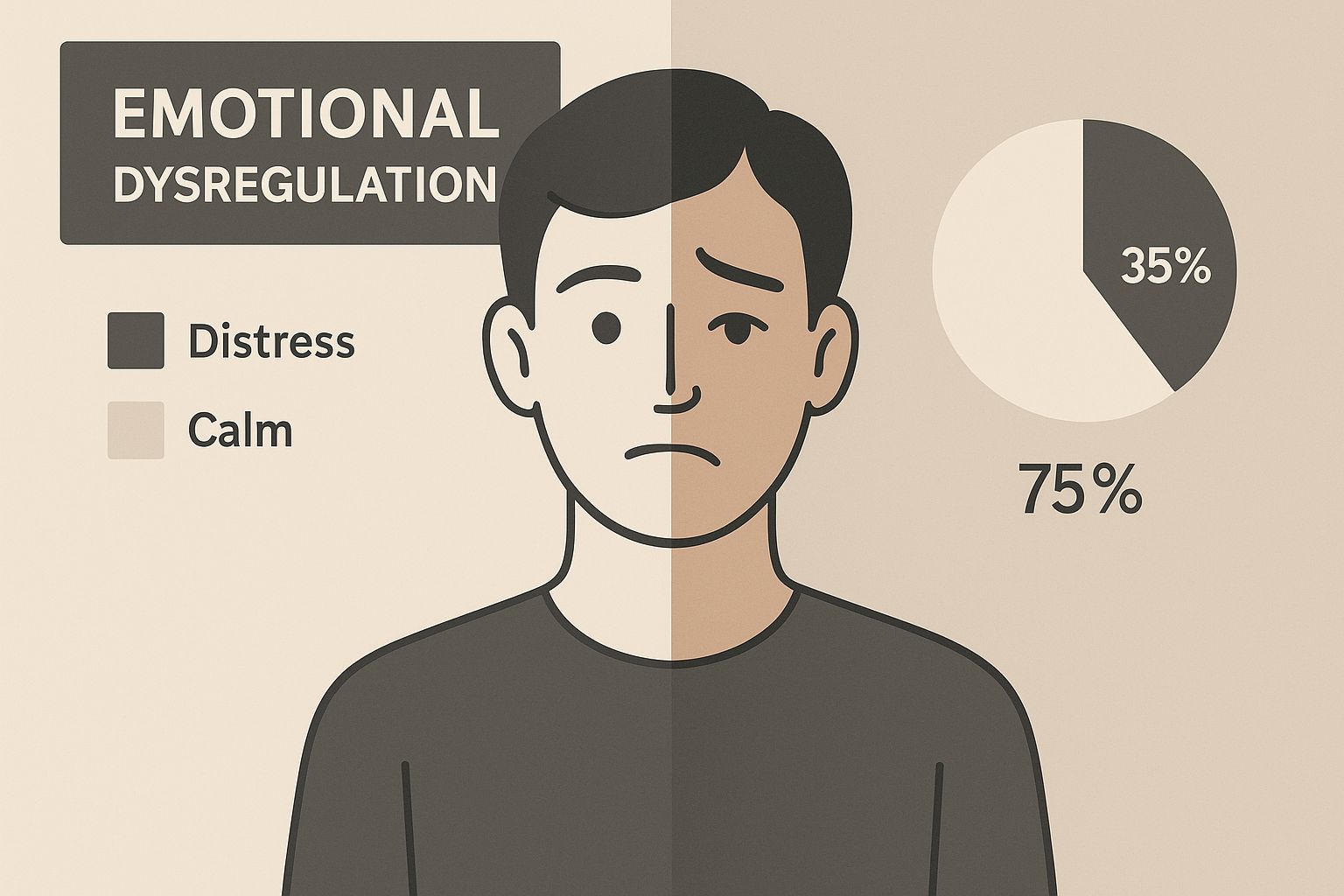
As the image shows, the emotional shifts in ADHD are often sharp, sudden, and completely invisible to others, which is a big part of what makes them so difficult to manage.
Why Your Brain Struggles with Emotional Control
To get to the bottom of why ADHD and mood swings go hand-in-hand, we have to look under the hood at the brain’s wiring. This isn't about willpower or character; it’s pure neurobiology. The intense emotional rollercoaster you might be feeling has a concrete explanation rooted in how your brain is built and how it communicates with itself.
At the heart of it all are two key brain regions: the prefrontal cortex (think of it as the brain's "mission control") and the limbic system (its "emotional core"). Your prefrontal cortex handles all the executive functions—things like impulse control, planning ahead, and putting the brakes on emotional reactions. The limbic system, on the other hand, is where raw emotions like fear, anger, and joy are born.
In a brain without ADHD, these two areas have a solid, reliable connection. Mission control keeps a steady hand on the emotional core, making sure reactions are balanced and appropriate for the situation.
But in the ADHD brain, that communication line can get fuzzy or drop out altogether. Imagine a skilled air traffic controller trying to guide a powerful jet, but their radio keeps crackling with static. The jet—your emotions—can suddenly swerve or take off without clear direction from the tower.
The Role of Brain Chemicals
This spotty connection is heavily influenced by neurotransmitters, the chemical messengers that carry signals across the brain. For ADHD, the most important player on the field is dopamine.
Dopamine is absolutely vital for managing attention, motivation, and our emotional responses. In the ADHD brain, the dopamine system just works differently, often resulting in lower or inconsistent levels of this critical chemical.
This dopamine deficit makes it incredibly hard for the prefrontal cortex to do its job. Without enough dopamine to power its circuits, "mission control" can’t effectively manage the intense signals firing from the emotional core. The result? Sudden, powerful mood swings that feel like they come out of nowhere.
Basically, the biological tools you need to tap the brakes on an emotional reaction just aren't always there when you need them. This can lead to what’s known as a dysregulated nervous system, where the body's entire stress-response system is thrown off balance.
Understanding this neurological foundation is the first real step toward getting a handle on these experiences. It helps shift the perspective from self-blame to self-awareness, giving you the power to find strategies that work with your brain's unique wiring instead of fighting against it.
Drawing the Line Between ADHD and Bipolar Disorder
The intense, roller-coaster nature of ADHD emotions often brings up a tough question: is this just ADHD, or could it be something else, like bipolar disorder? It’s an easy mistake to make, since both conditions involve major mood shifts. But if you look closer, you’ll see the triggers, timing, and underlying reasons are worlds apart.
Getting this distinction right is absolutely essential. The right diagnosis leads to the right treatment, but getting it wrong can mean years of frustration and feeling like you’re getting nowhere. The key is to pay attention to the pattern of the mood swings—how they start, how long they last, and what sets them off.
Understanding the Triggers and Timing
One of the best ways I've found to explain the difference is by using a weather analogy. Think of ADHD mood swings as reactive—like a flash flood. They’re almost always sparked by something happening right now: a comment you take as rejection, a frustrating mistake at work, or just too much noise in a crowded room. The emotion hits hard and fast, but it can disappear just as quickly once the trigger is gone or your attention gets pulled elsewhere.
Bipolar disorder, on the other hand, operates on a much longer cycle. Its mood episodes are more like emotional seasons. We’re talking about prolonged periods of depression or mania (or the less intense hypomania) that can last for days, weeks, or even months. These episodes aren't just a reaction to a bad day; they're driven by internal shifts in brain chemistry and aren't tied to a specific, momentary event.
The core difference lies in their nature: ADHD mood swings are a rapid reaction to the immediate environment, while bipolar episodes are sustained, internally driven mood states that dramatically alter a person's entire experience of life for an extended period.
Making this distinction is even more important because the two conditions can, and often do, show up together. In fact, research shows a pretty significant overlap. One major study found that while bipolar disorder is relatively rare in the general population (affecting 0.2% to 3.6%), it’s found in anywhere from 4.48% to 35.3% of people with ADHD. You can dive deeper into the connection between ADHD and mood disorders in this detailed analysis.
To make it even clearer, here’s a quick breakdown of the key differences:
- Duration of Moods: With ADHD, your mood can swing wildly multiple times in a single afternoon. Bipolar episodes are sustained for at least several days (for hypomania) or a week or more (for mania).
- Cause of Moods: ADHD mood swings are almost always a direct, immediate reaction to a trigger. Bipolar mood episodes often seem to come out of the blue, without a clear external cause.
- Consistency: The emotional dysregulation of ADHD is a constant, day-in-day-out part of the experience. Bipolar disorder involves distinct episodes of depression and mania, often separated by periods of a more stable mood.
Understanding Co-Occurring Mood Disorders
ADHD rarely travels alone. In fact, it very often shares the stage with other conditions, especially mood disorders like anxiety and depression. This creates a complex picture of emotional health that can be tricky to sort out.
This overlap isn't just a coincidence; it’s rooted in a combination of shared brain wiring and the simple, grinding exhaustion that comes with living with ADHD. Constantly battling to focus, manage impulses, and stay organized in a world not built for your brain is incredibly stressful. This chronic stress can create a damaging cycle of perceived failure and low self-esteem, laying the groundwork for a mood disorder to take hold.
The High Rate of Comorbidity
The connection is so strong that having more than one diagnosis is really more the rule than the exception. For treatment to be effective, it often means addressing both conditions at the same time, since they can easily amplify each other's symptoms. Think about it: the worry from an anxiety disorder can make ADHD-related inattention even worse.
This is exactly why a comprehensive diagnosis is so important. Research shows that about 38% of adults with ADHD also have a co-occurring mood disorder. Digging deeper, nearly 47% live with a depressive disorder, while up to 20% experience symptoms of bipolar disorder. You can learn more about these coexisting conditions from CHADD, a fantastic resource.
Understanding this high rate of comorbidity is the first step toward destigmatizing the experience. It confirms that you are not alone in managing these layered challenges and highlights the need for a care plan that addresses your whole mental health picture.
Managing these overlapping conditions can feel overwhelming, but many people find that addressing the underlying stress and nervous system dysregulation is key. For those exploring different avenues for wellness, it can be helpful to read our guide on chiropractic care for anxiety and depression.
Actionable Strategies for Managing Mood Swings

Knowing why ADHD can lead to mood swings is one thing; learning what to do about them is the real game-changer. While you can't just rewire your brain on command, you can absolutely build a powerful toolkit of strategies that work with your unique neurobiology, not against it.
This isn't about ignoring your feelings or pretending they don't exist. It's about learning to navigate the emotional currents without letting them pull you under. The goal is to create just enough space between a trigger and your reaction, giving you a chance to respond thoughtfully instead of getting swept away by an emotional flash flood.
Behavioral and Mindfulness Techniques
You can't manage an emotional surge if you don't see it coming. This is where mindfulness comes in. It's like training your brain's internal weather forecaster to spot the signs of a storm before it hits.
A surprisingly simple but powerful technique is called “Name It to Tame It.” The moment you feel a big emotion bubbling up—frustration, anger, overwhelm—just pause and put a label on it. Simply thinking, "Okay, this is frustration," can feel like flipping a switch. It brings your prefrontal cortex, the brain's "mission control," back online to help you manage the emotional static.
By simply putting a name to a powerful feeling, you shift from being consumed by it to observing it. This small step creates just enough distance to prevent an impulsive overreaction and regain a sense of control.
Lifestyle Adjustments for Brain Health
Often, the strongest foundation for emotional stability is built on simple, daily habits. For the ADHD brain, a few key areas can make a world of difference in keeping mood swings in check.
- Consistent Sleep: Think of sleep as a nightly reset button for your prefrontal cortex. When you don't get enough, your brain's emotional regulation center is already running on fumes, making you far more susceptible to dysregulation.
- Brain-Boosting Nutrition: Your brain needs the right fuel. Foods high in protein and omega-3s help support the dopamine pathways that are so crucial for ADHD. On the flip side, loading up on sugar and simple carbs can lead to energy crashes that only make irritability worse.
- Regular Exercise: Moving your body is one of the most effective, non-pharmaceutical ways to boost dopamine and norepinephrine—the very neurotransmitters that ADHD medication targets. Even a brisk 20-minute walk can have a powerful calming and focusing effect.
Professional Support and Therapies
While self-management skills are your first line of defense, professional guidance can offer a structured path and expert insights. Therapies like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) have been proven incredibly effective, especially when adapted for the ADHD mind.
CBT is fantastic for helping you spot and challenge the negative thought patterns that often act as triggers for intense emotions. DBT, on the other hand, is all about building practical skills in mindfulness, distress tolerance, and emotional regulation. A good therapist acts as a coach, helping you build a personalized playbook that combines these tools with lifestyle changes to effectively manage the emotional side of ADHD.
Frequently Asked Questions About ADHD and Moods
When you start digging into the connection between ADHD and emotional health, a lot of specific questions tend to pop up. Let's walk through some of the most common concerns with clear, straightforward answers to help you better understand the nuances of how ADHD can impact mood.
Can ADHD Medication Help With Mood Swings?
Yes, for many people, the right ADHD medication can be a total game-changer for emotional regulation. Both stimulant and non-stimulant medications work by improving the communication pathways in the brain, especially those that rely on dopamine and norepinephrine.
Think of the prefrontal cortex as your brain's "mission control." By boosting these pathways, medication helps it do its job better—managing impulses and emotional reactions. As a result, many people find their irritability and reactivity decrease. This gives them that crucial split-second of mental space to respond thoughtfully instead of just reacting. Of course, medication almost always works best when it's part of a bigger plan that includes therapy and lifestyle adjustments.
What Is Rejection Sensitive Dysphoria (RSD)?
Rejection Sensitive Dysphoria (RSD) is a term that perfectly describes an extreme emotional sensitivity and pain triggered by the perception of being rejected or criticized. While it isn't an official diagnosis in the DSM, it powerfully captures a very real and common experience for those with ADHD.
With RSD, a minor comment or a simple misunderstanding can feel like a devastating personal attack. It can trigger an overwhelming and immediate flood of hurt, anger, or sadness. This is a perfect example of how ADHD can cause mood swings by turning up the volume on emotional responses to social situations.
How Do I Know if My Child's Moodiness Is ADHD?
Distinguishing typical childhood moodiness from ADHD-related emotional dysregulation really comes down to three things: intensity, frequency, and recovery time. A typical kid might get upset, sulk for a bit, and then move on.
An ADHD-related emotional outburst, on the other hand, is often like a firework—it explodes with incredible intensity but can be over just as quickly. If your child’s mood swings are extreme, happening all the time, and consistently getting in the way of their ability to succeed at school or keep friends, that’s a strong sign it's time to seek a professional evaluation.
At First Steps Chiropractic, we focus on optimizing nervous system function to help families find balance and resilience. Schedule a complimentary consultation with us today.

