If you're a parent of an autistic child and you've noticed that night terrors seem to happen a lot more frequently, you're not alone. It's a real connection. The link between autism and night terrors often comes down to fundamental differences in nervous system regulation, sensory processing, and higher levels of anxiety.
All these factors can make it harder for the brain to transition smoothly between sleep stages, creating the perfect storm for these jarring episodes.
Unpacking the Connection Between Autism and Sleep
Witnessing your child in the middle of a night terror is a truly unsettling experience. The sudden screaming, the thrashing, and the look of sheer terror are alarming, especially when your child seems completely unaware of you. It’s scary, but understanding what’s happening can bring a sense of clarity and calm.
Think of the brain’s sleep-wake cycle not as a smooth dimmer switch, but as one that sometimes flickers and shorts out. This causes a sudden, confusing partial arousal from the deepest stage of sleep—and that’s a night terror.
An autistic child’s unique neurobiology is right at the center of this. Their nervous systems are often wired to be far more sensitive and can get overwhelmed by the sensory input of a typical day. This can leave them in a state of high alert, making it difficult for their brain and body to fully power down and get truly restful sleep. You can learn more about how this works in our guide to autism and the nervous system.
Distinguishing Night Terrors from Nightmares
One of the most important first steps for any parent is learning to tell the difference between a night terror and a regular nightmare. Your response needs to be completely different for each. Comforting a child during a nightmare is exactly what you should do, but trying to wake them from a night terror can actually make the episode longer and more intense.
While night terrors are pretty rare in the general population, affecting about 1% to 6.5% of children, the numbers are much higher in the autistic community. Broader studies on Disorders of Partial Arousal (which include night terrors) show rates as high as 29.4% in autistic children. This highlights a clear neurological link.
To help you tell them apart, here's a quick comparison.
Night Terror vs Nightmare Key Differences
This table breaks down the key differences between these two sleep events, helping you know what to look for so you can respond in the most helpful way.
| Characteristic | Night Terror (Parasomnia) | Nightmare |
|---|---|---|
| State of Awareness | Child is asleep and unaware of surroundings. | Child is fully awake after the dream. |
| Responsiveness | Unresponsive, cannot be woken or comforted. | Responds to comfort and can be soothed. |
| Memory of Event | No memory of the episode the next day. | Can often recall parts of the bad dream. |
| Physical Signs | Screaming, thrashing, sweating, wide-eyed stare. | Crying, fear, seeking parental comfort. |
| Timing | Typically occurs in the first third of the night. | Usually happens in the early morning hours. |
The key takeaway is that during a night terror, the child remains completely asleep and has no idea what’s happening or that you're even there. The next day, they won't remember a thing.
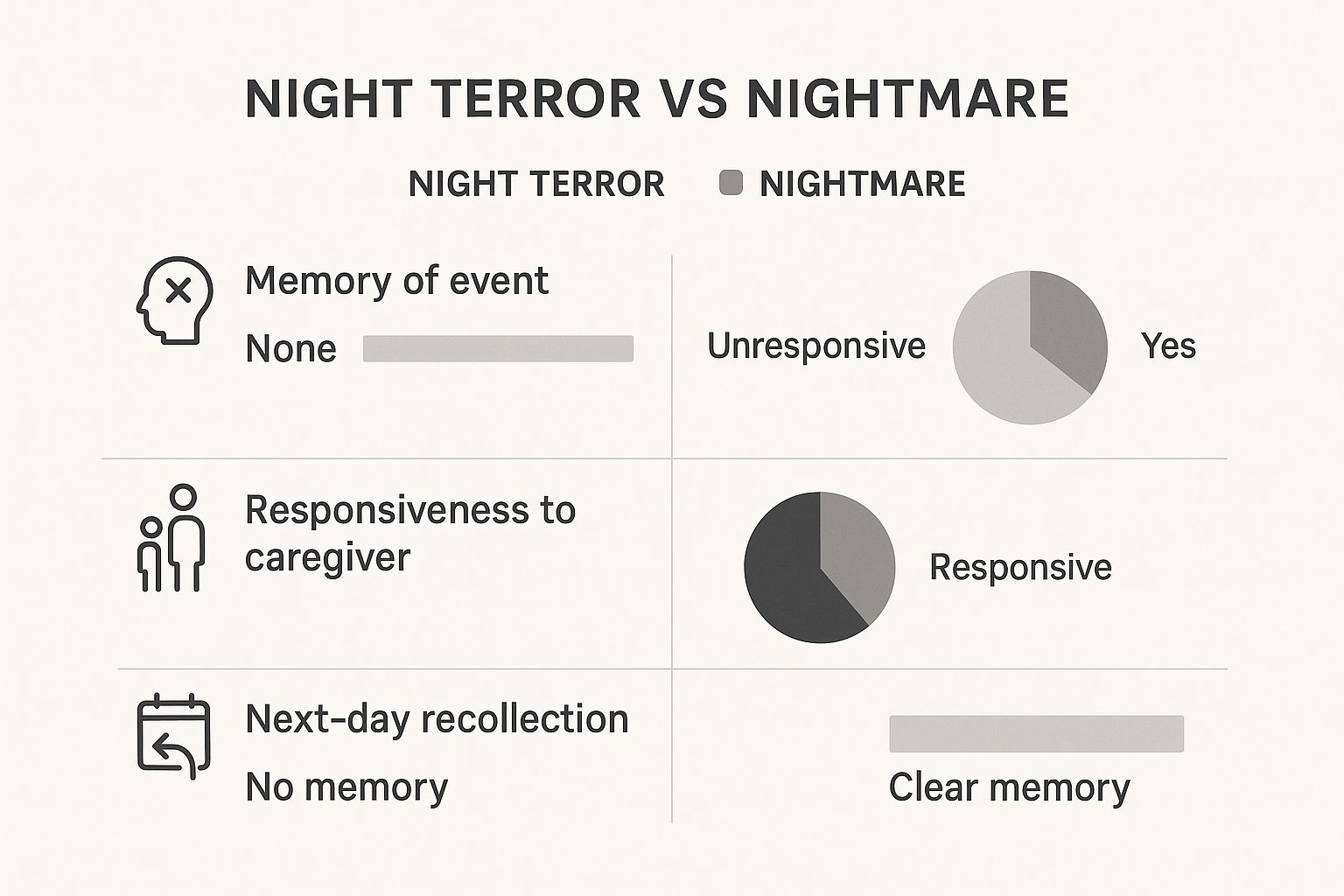
This is the complete opposite of a nightmare, where a child is often relieved to be woken up and can tell you about the scary dream. Recognizing these signs helps you stay calm and focus on the one thing that truly matters: keeping your child safe until the episode passes on its own.
Why Night Terrors Are More Common in Autistic Children
The higher frequency of night terrors in autistic children isn't just a coincidence; it's deeply connected to some very real neurological and physiological differences. Once you understand the underlying reasons, it’s easier to see these episodes not as a behavioral problem, but as the body's physical response to being overwhelmed.
Think of a child's nervous system like a bucket that gets filled with sensory information all day long. For an autistic child, that bucket is often filled much faster by bright lights, constant background noise, and the sheer effort of social interactions. By bedtime, that bucket isn't just full—it's overflowing, making it incredibly difficult for their brain and body to power down and shift into a state of deep, restorative rest.
The Role of Sensory Overload
An autistic child’s brain often processes the world with the volume turned way up. A sound that might be a minor annoyance to a neurotypical person can feel like a blaring alarm bell to them. This heightened sensitivity means their nervous system spends much of the day in a state of high alert.
This build-up of sensory stress doesn’t just vanish when the lights go out. It can linger, keeping the brain in a dysregulated state and making the delicate transitions between sleep stages much more turbulent. The brain essentially gets "stuck" and struggles to settle into deep sleep, creating the perfect opening for a partial arousal—a night terror—to burst through.

Heightened Anxiety and the Fight-or-Flight Response
Anxiety is a very common co-occurring condition with autism, and it's a major player when it comes to sleep problems. Anxiety keeps the body’s sympathetic nervous system—our internal "fight-or-flight" alarm—switched on, even during sleep.
When this system stays on high alert, the body remains tense and the brain stays vigilant for threats. This underlying state of stress is like a coiled spring, ready to trigger the sudden, panicked reactions we see in a night terror. The body is essentially primed for a major fear response, even when there's no actual danger.
Night terrors are a physiological event, not a conscious choice or a sign of bad behavior. They represent the nervous system's struggle to downshift from a day of overwhelming input and heightened anxiety into a state of deep, restorative sleep.
Differences in Sleep Architecture
Finally, we have to look at the very structure of sleep itself, which can be quite different for autistic individuals. Research consistently shows that they face significant challenges with sleep patterns, which affects the natural flow through the different sleep cycles. And these aren't minor issues—studies suggest that anywhere from 50–80% of autistic children experience significant sleep problems. You can dig into the research on autism and sleep disturbances here for a deeper look.
This difficulty in maintaining a stable sleep cycle is key. Night terrors happen specifically during the transition out of non-REM sleep, which is the deepest stage. If the brain’s ability to navigate that transition is impaired, it's like a car lurching and jolting as it tries to shift gears. For an autistic child, that neurological "jolt" can manifest as a terrifying but completely unconscious episode, leaving parents to manage the aftermath.
How to Recognize a Night Terror in Your Child
When a night terror hits, it's nothing short of chaotic and terrifying, especially for a parent witnessing it for the first time. Knowing what you’re looking at is the first step toward responding effectively, rather than reacting out of pure fear.
The signs are very different from a typical nightmare, and being able to spot them helps you keep your child safe until the episode is over.
A night terror isn’t just a bad dream. It’s a sudden, partial arousal from the deepest stage of non-REM sleep. The most jarring sign for parents is that your child will look like they're awake, but they absolutely aren’t.
Their eyes might be wide open with a glassy, unfocused stare, looking right through you without a hint of recognition. This is one of the clearest signs that they are still completely asleep.
Common Signs to Watch For
During an episode, you’ll likely see a combination of intense physical and vocal reactions. It’s important to remember your child has no control over these actions and will have zero memory of them in the morning.
- Sudden, Loud Vocalizations: This can be anything from blood-curdling screams and shouting words that don't make sense to gasping for air in terror.
- Intense Physical Movement: You might see them thrashing around, kicking, or flailing in bed. Some kids even bolt upright or try to climb out of bed, which is a major safety concern.
- Signs of Panic: Look for physical signs of the body’s fight-or-flight system kicking in—a racing heart, rapid breathing, sweating, and flushed skin.
- Inconsolable State: Trying to hold, hug, or comfort your child will probably have no effect. In fact, it might make the episode even more intense because they aren't consciously aware you're even there.
The Impact of Sensory Needs
For an autistic child, their unique sensory profile can really shape what the night terror looks like. A child who is hypersensitive to touch might react even more intensely if you try to hold them, perceiving that contact as an overwhelming threat instead of comfort.
They are not rejecting you. Their sleeping brain is simply reacting to sensory input that it can’t process in that moment.
The most crucial thing to remember is that your child is completely asleep during a night terror. They are not aware of what is happening and will have no memory of the event the next morning. Your role is not to wake them, but to ensure their physical safety.
Learning to recognize these signs helps you stay calm and shift your focus. Instead of trying to stop the event, you become a quiet guardian. The goal is simply to prevent accidental injury from the thrashing until their brain naturally transitions back to a calmer state of sleep. Your quiet, protective presence is the best support you can offer.
Actionable Strategies for Reducing Night Terrors

When you're trying to manage the connection between autism and night terrors, the goal is to play the long game. It's less about stopping an episode as it's happening—which is often impossible—and more about creating an environment where they happen less often and with less intensity. These proactive, compassionate strategies are all designed to support your child’s nervous system.
Think of it like building a gentle off-ramp from the day’s constant stream of stimulation. A predictable, sensory-friendly bedtime routine is your single most powerful tool. This ritual sends clear signals to the brain and body that it's time to shift gears and wind down, which is crucial for easing the transition into the deep sleep stages where night terrors live.
Consistency is everything here. An overtired brain is far more likely to experience sleep disruptions. A strict sleep schedule helps regulate the body’s internal clock, preventing the kind of deep sleep deprivation that so often pulls the trigger on these frightening episodes.
Create a Sensory-Friendly Sleep Sanctuary
A child's bedroom can either be a source of calm or a source of agitation for a sensitive nervous system. Your mission is to transform it into a "sleep sanctuary" by swapping out jarring sensory input for predictable, soothing sensations that invite rest.
This is the perfect place to bring in a pre-sleep "sensory diet" that's tailored to your child’s specific needs. Some ideas might include:
- Deep Pressure: A weighted blanket or even just a gentle massage before lights-out can have a profoundly calming effect on the nervous system.
- Auditory Regulation: White noise machines or a simple fan are great for masking sudden household sounds that could otherwise startle them and disrupt a sleep cycle.
- Visual Calm: Blackout curtains are a game-changer. Creating a truly dark environment helps trigger the production of melatonin, the body's natural sleep hormone.
- Tactile Comfort: Don't overlook the little things. Soft, seamless pajamas and cozy bedding can make a huge difference by reducing any tactile irritation that leads to restlessness.
By carefully curating the sensory environment, you help lower the overall stress load on your child's system. This makes the journey into peaceful sleep much smoother. If you want to dive deeper into how sensory inputs affect the body, you can read more about how to repair your autonomic nervous system.
The Power of Predictability and Routine
For any child, but especially an autistic child, predictability equals safety. A consistent bedtime routine is like a roadmap for the brain, guiding it step-by-step from a state of high alert to one of rest and calm. The routine should be simple, relaxing, and—most importantly—done in the exact same order every single night.
A great routine might look something like this:
- Dim the Lights: About an hour before bedtime, lower the lights throughout the house. This is a powerful, non-verbal cue that the day is ending.
- Quiet Down: Switch from stimulating activities like screen time to quiet ones. Think reading a book together or listening to some calm, ambient music.
- Warm Bath: A warm bath is fantastic for relaxing tense muscles. The gentle drop in body temperature after getting out also naturally signals the body that it's time for sleep.
- Final Connection: Spend the last few minutes in their room with them, just being present. This offers a final dose of security and connection right before they drift off.
The consistency of a bedtime routine does more than just prepare a child for sleep; it helps regulate their entire nervous system. It provides a predictable structure that reduces anxiety and makes the brain feel safe enough to fully disengage and enter deep, restorative sleep stages.
Remember, these are just starting points. The key is to observe your child. Pay attention to what soothes their system and what seems to wind them up. Finding that unique combination of sensory support and routine is what will ultimately pave the way for more peaceful nights.
How Gentle Chiropractic Care Can Support Sleep

While building sensory-friendly routines is a cornerstone for managing the connection between autism and night terrors, many parents also look for complementary ways to support their child’s nervous system directly. This is where gentle, neurologically-focused chiropractic care comes in. It’s an approach designed to get to the root of the neurological stress that can fuel these sleep disruptions.
The central idea is to help a child’s body shift out of that constant, wound-up "fight-or-flight" mode. Imagine a nervous system that’s stuck in the “on” position, buzzing with high alert all day long. This state, which we call sympathetic dominance, makes it incredibly hard for a child to wind down and get the deep, restorative sleep they need to prevent those jarring partial arousals.
Easing the Body into a State of Rest
When we talk about gentle chiropractic adjustments, we’re not talking about forceful movements. It’s all about providing precise, light input to the nervous system. The goal is to reduce interference so the body can more easily switch into the parasympathetic state—that wonderful "rest and digest" mode where real relaxation and healing happen.
By calming this built-up neurological tension, the body can navigate the transitions between sleep stages more smoothly. For many kids, this means fewer abrupt awakenings and a noticeable reduction in how often—and how intensely—night terrors happen.
This supportive therapy isn’t a replacement for other strategies like good sleep hygiene and sensory regulation. Instead, it works alongside them, helping the body’s internal communication system run more efficiently and making it easier for a child to find a true state of calm.
A Holistic Approach to Wellness
Looking at sleep issues through a neurological lens gives parents another powerful tool. It complements everything else you’re doing by focusing on the body’s innate ability to regulate itself once that neurological interference is dialed down.
This approach helps create a foundation of neurological balance that supports not just better sleep, but a child’s overall well-being. To learn more about how this works, you can read our detailed guide on autism and chiropractic care.
When to Seek Professional Support for Sleep Problems
While so many strategies for managing autism and night terrors can be put into practice at home, it's absolutely vital to recognize when you need to call in an expert. Trying to handle everything on your own, especially when the episodes are severe or frequent, is a fast track to burnout.
Knowing the signs that it’s time to ask for help is one of the most important ways you can advocate for your child. Your home strategies are the foundation, but sometimes there's a deeper issue that requires a specialist's eye.
If night terrors start happening more often, last longer, or involve intense or potentially dangerous movements, that’s a clear signal. Your child's safety is always priority number one.
You also want to pay close attention to how they are the next day. Is the disrupted sleep causing significant daytime fatigue? Is it making it hard for your child to participate in school, therapy, or just daily family life? If so, it’s time for professional intervention. Sleep isn't a luxury—it’s essential for development, learning, and regulation.
Identifying the Right Professionals to Help
Navigating the healthcare system can feel overwhelming, but knowing who to turn to gives you a clear roadmap forward. The right expert can offer targeted support that works hand-in-hand with the calming, supportive environment you’ve already built at home.
Here are a few of the specialists who can provide incredible assistance:
- Developmental Pediatrician: This is a doctor who specializes in the development of children with neurodevelopmental differences. They can help rule out any underlying medical issues that might be contributing to the sleep challenges.
- Sleep Consultant or Specialist: A sleep expert can conduct a thorough evaluation, sometimes including a sleep study, to get a precise picture of what’s happening during the night. This data can be invaluable.
- Occupational Therapist (OT): An OT is a fantastic resource for addressing the sensory processing challenges that often fuel night terrors. They can help you create a more effective "sensory diet" for your child to promote better regulation day and night.
Reaching out for professional support is not a sign of failure; it is a proactive step toward ensuring your child and family have the comprehensive care needed to thrive. It empowers you with a team of experts dedicated to finding solutions.
Ultimately, if the stress of managing these episodes becomes overwhelming for you and your family, that in itself is a perfectly valid reason to seek support. A professional can provide not just strategies for your child, but also guidance and reassurance for you as the caregiver. You don't have to do this alone.
When you're trying to connect the dots between autism and night terrors, it's natural to have a lot of questions. This last section is all about giving you direct, clear answers to the most common things parents worry about.
Our goal is to clear up any lingering doubts so you feel more confident and prepared to support your child through these tough nights.
Can My Child Get Hurt During a Night Terror?
Even though your child is completely unaware of what’s happening, the intense physical thrashing during an episode can absolutely pose a risk of injury. Because of this, safety has to be your number one priority.
Take a look around their sleep area and clear out anything with sharp corners or hard surfaces. It’s also a good idea to secure windows and maybe even put a mattress on the floor if the thrashing is particularly severe. The key isn't to stop the episode—it's to create a safe cocoon where it can run its course without any bumps or bruises.
Will My Autistic Child Outgrow Night Terrors?
For many kids, both neurotypical and autistic, night terrors do fade away as their nervous systems develop and mature. That said, it's crucial to remember the strong link between these episodes and the core traits of autism.
Because sleep issues are often connected to ongoing challenges with sensory sensitivities and anxiety, proactive strategies for sleep hygiene and nervous system regulation remain essential for providing long-term support, even as they get older.
Should I Tell My Child About Their Night Terrors?
As a general rule, it’s best not to discuss the night terror with your child. They have absolutely no memory of it, so bringing it up is far more likely to cause unnecessary anxiety or fear about bedtime than to actually help.
Instead of talking about the episode itself, channel your energy into maintaining a positive, predictable, and calming bedtime routine. This builds a feeling of security that works wonders for their nervous system.
At First Steps Chiropractic, we see the deep connection between a regulated nervous system and truly restorative sleep every single day. If you're looking for gentle, neurologically-focused support to help your child find calmer nights, we invite you to learn more about our approach. Explore how we can help your family by visiting us at https://firststepschiropractic.com.

