When families first learn about the low muscle tone autism spectrum connection, it often clicks into place. This isn't just some secondary issue; it's a deeply intertwined part of the picture. Hypotonia, the clinical term for low muscle tone, is a very common co-occurring condition in autism, shaping everything from motor skills and posture to coordination. It’s not just a physical trait—it's a key aspect of the unique neurodevelopment we see in so many incredible kids on the spectrum.
Unpacking the Link Between Hypotonia and Autism

So, how does this connection actually work?
Think of the nervous system as the body's internal wiring and the muscles as light bulbs. For the lights to shine brightly and consistently, they need a steady, strong electrical signal. If that signal is weak or inconsistent, the bulbs might flicker or just stay dim.
In a similar way, when an autistic child's nervous system has communication challenges, the signals telling the muscles how to contract and maintain their resting state can get a bit jumbled. This doesn't mean the muscles are weak; it means the baseline tension in them is low.
The result is muscles that can appear "floppy" or less firm than you'd expect. That's hypotonia. It's not a strength problem, but an issue with the nervous system's ability to keep the muscles in a ready state.
Research shows just how common this is. It's estimated that approximately 50% of children with autism spectrum disorder (ASD) have low muscle tone, a rate that’s way higher than in the general pediatric population. You can dive deeper into this connection over at PXDocs.
Quick Guide to Hypotonia Signs in Children with ASD
For parents and caregivers, knowing what to look for can make a huge difference. This table breaks down some of the common signs of low muscle tone, from observable physical traits to specific motor skill challenges.
| Physical Signs | Motor Skill Challenges |
|---|---|
| "Floppy" or rag-doll-like limbs | Delays in hitting milestones (sitting up, crawling, walking) |
| Poor head control, especially in infants | Difficulty with fine motor tasks like holding a pencil or using scissors |
| Hypermobile or overly flexible joints | Clumsiness or frequent falling |
| Tendency to lean on furniture or people for support | Trouble with activities requiring endurance, like running or climbing |
| Slumped posture when sitting or standing | Challenges with tasks requiring core strength, like sitting upright |
Recognizing these signs early allows for proactive support, helping kids build the foundational strength and coordination they need to thrive.
Why This Connection Matters for Development
The presence of low muscle tone can create a ripple effect across a child's development, introducing hurdles that go way beyond just physical movement. These difficulties often intersect with—and can even amplify—the core challenges that come with autism.
Here’s what that can look like:
- Motor Skill Delays: Little ones might struggle with major milestones like sitting up on their own, crawling, or taking their first steps. Even fine motor skills, like learning to hold a crayon or buttoning a shirt, can feel like a monumental task.
- Postural Instability: A weak core makes everything harder. It can be exhausting for a child to simply sit upright at a desk or on the floor during circle time, which can impact their ability to focus and learn.
- Reduced Endurance: Kids with hypotonia often get tired much more quickly than their peers. This can limit their participation in playground fun, sports, and even classroom activities that require sustained physical effort.
When we view low muscle tone not as an isolated problem but as a direct manifestation of a child's unique neurology, we can start to see the bigger picture. Addressing these motor challenges isn't just about physical therapy; it's a fundamental part of a holistic approach to autism care that helps children build confidence and engage more fully with the world around them.
How to Recognize the Signs of Hypotonia
Spotting the signs of low muscle tone, or hypotonia, is the first and most critical step for parents. These clues can be subtle, often blending in with a child's unique development, but catching them early can make all the difference. Instead of getting bogged down in clinical jargon, let’s talk about what these signs actually look like day-to-day.
With infants, you might hear parents use terms like "floppy" or "rag-doll" to describe how their baby feels when they're picked up. They just don't feel as firm, and they might have a tough time holding their head up on their own. This isn't about weakness; it's that their muscles aren't in a state of "ready" like you'd typically expect.
As kids get a bit older, the signs of low muscle tone autism spectrum can show up in how they move and hold themselves. You may notice your toddler slumps when they sit or seems to rely on furniture for support way more than other kids their age.
Gross Motor Skill Indicators
Gross motor skills are the big movements—walking, running, jumping. For a child with hypotonia, these skills can take longer to master or just look a bit clumsy and uncoordinated.
Here are a few common things to watch for:
- Delayed Milestones: They might be a little behind on the big physical achievements, like sitting up without help, crawling, or taking those first steps.
- Clumsiness: Does your child frequently trip over their own feet or bump into things? This general lack of coordination during play can be a sign.
- Low Endurance: They seem to get tired out much more quickly than their friends during a trip to the park or just playing in the backyard.
- Unusual Gait: You might notice they walk with their feet spread wide to stay balanced or have a bit of a "waddle" in their step.
These motor challenges are often tied to how a child's brain is processing sensory information. To see how deeply connected these systems are, it helps to understand what sensory processing disorder is and the role it plays in movement and coordination.
Fine Motor Skill Difficulties
Hypotonia doesn't just affect the big muscles; it also impacts the small, precise muscles in the hands and fingers. These fine motor challenges can be a huge source of frustration for kids who are just trying to keep up at home and in school.
A child with low muscle tone might have to work significantly harder just to hold a pencil correctly, which can make learning to write feel like an exhausting chore instead of a creative outlet. This extra effort can impact their confidence and willingness to engage in academic tasks.
Keep an eye out for these specific fine motor signs:
- A Weak Grasp: They may have a hard time holding onto crayons, forks, or small toys.
- Trouble with Fasteners: Buttons, zippers, and snaps can remain a major challenge long after their peers have figured them out.
- Messy Handwriting: Their writing might be large, sloppy, and all over the place because controlling the pencil is so difficult.
- Difficulty with Manipulation: Tasks like using scissors, building with LEGOs, or stringing beads can be tough.
Recognizing these signs isn't about putting a label on your child. It's about truly understanding their unique physical needs. Once you see these hurdles for what they are, you can start finding supportive strategies to help them build strength, coordination, and—most importantly—the confidence to navigate their world.
Why Hypotonia Can Be an Early Clue for Autism

When a new baby arrives, parents are often focused on hitting those big, visible milestones—the first smile, the first coo, and eventually, crawling and walking. While these achievements might seem unrelated, they're all outward signs of a brain and nervous system that are developing at an incredible pace. Motor skills, in particular, give us one of the earliest and clearest glimpses into this amazing connection.
That’s why challenges with motor control can be such a valuable window into a child's neurological journey. Think of it like building a new house. Long before the walls are painted, you see the foundational framework and all the wiring being laid. Motor skills are a lot like that foundational framework for the body. If there are early difficulties here, it can sometimes signal that the underlying "wiring"—the nervous system—is developing in a unique way.
This is exactly why the link between low muscle tone and the autism spectrum is so important for parents to understand. Hypotonia is so much more than just “floppy” arms and legs. It’s a physical clue that can point toward broader neurodevelopmental patterns, reflecting how a child’s brain is processing signals and coordinating movement right from the start.
The Research Backing Early Detection
A growing body of research is confirming what many practitioners have observed for years: early motor challenges can often be a precursor to a later autism diagnosis. This doesn’t mean every child with low muscle tone is on the spectrum, but it does highlight a strong correlation that is too significant to ignore. Seeing this connection gives parents and providers a crucial opportunity for earlier awareness and support.
Hypotonia in infancy can be more than just a motor delay; it can be one of the first visible indicators of the unique neurodevelopmental path associated with autism, prompting a closer look at a child's overall developmental trajectory.
One major population-based study followed 2,905 children from infancy through their early years. The results were clear, showing that hypotonia in infancy was a significant predictor of higher autistic traits later on. This suggests that low muscle tone could serve as an important early biomarker. You can dive deeper into this groundbreaking research on PMC.
Empowering Parents with Knowledge
Understanding this connection is incredibly empowering. It allows you to become a proactive advocate for your child’s health and well-being. If you notice signs of low muscle tone, you can bring these specific observations to your pediatrician and ask for a comprehensive developmental screening. This knowledge helps shift the conversation from a passive "let's wait and see" approach to a proactive "let's investigate and support" mindset.
Identifying motor delays early can open the door to supportive therapies that help children build strength, coordination, and confidence. It also encourages a more holistic assessment of a child’s development, ensuring they get the right support at the right time. Exploring comprehensive care is a vital part of this journey, and you can learn more about holistic approaches to autism in our dedicated blog post.
How Hypotonia Shapes a Child's Development
Low muscle tone creates a ripple effect that touches nearly every part of a child's growth and development. Imagine trying to build a house on a foundation that’s just a bit wobbly. It’s not impossible, but every single step requires more work, more concentration, and more energy. For a child with hypotonia, that’s what everyday movement feels like.
When a child’s muscles don’t have that ready-to-go tension, even simple actions like sitting up straight or reaching for a toy become a monumental effort. This constant physical struggle naturally shapes how they experience and interact with the world around them. The challenges go far beyond just delayed milestones like walking or running; they color a child's ability to explore, learn, and play.
The Connection to Earlier Diagnosis
Interestingly, a child’s motor difficulties can sometimes be the very thing that leads to an earlier autism diagnosis. While that might sound backward, it makes sense when you think about it. When parents see very clear, observable physical challenges, they are often prompted to seek developmental assessments sooner than they might have otherwise.
This link really highlights just how deeply our motor and neurological systems are intertwined.
A child’s physical development is often one of the first and most visible signs parents notice. When something seems off, it can serve as a red flag that encourages a deeper look into their overall neurodevelopment, which can speed up the identification of autism and get supportive care started.
In fact, research with infants has shown that low muscle tone is a significant factor in getting an earlier diagnosis. For baby boys, hypotonia was linked to an average acceleration of diagnosis by 1.5 years. For girls, the acceleration was about one year. You can dive deeper into these findings in the full research study.
The Broader Developmental Impact
The impact of low muscle tone within the autism spectrum is about so much more than just the physical. These motor challenges can have significant emotional and cognitive consequences, directly influencing a child's self-esteem and their progress in school.
Here’s how these physical struggles can show up in other areas of life:
- Social Participation: When a child can't physically keep up on the playground, they may start to feel left out. This can lead to social isolation or a preference for sitting alone with a book or a screen instead of joining in.
- Academic Engagement: Think about the sheer physical effort it takes for them just to sit still at a desk, hold a pencil correctly, and keep their head up. This can be exhausting, leaving very little mental energy for the actual learning part.
- Self-Esteem and Confidence: Constantly struggling with tasks that seem to come so easily to their peers can take a huge toll. It can really knock down a child's confidence and make them hesitant to try new things.
Tackling these motor challenges isn't just about building up strength. It's a critical piece of the autism care puzzle. By supporting their physical foundation, we help them engage more confidently and successfully with their entire world.
Supportive Therapies for Low Muscle Tone
Once you understand the physical hurdles that come with low muscle tone, the next step is finding the right support. The most effective strategy is almost always a team effort, bringing together different specialists who can tackle the unique ways hypotonia affects a child's development. This isn't about "fixing" anything; it's about empowerment.
These therapies give kids the tools, strength, and coordination to move through their world with more confidence and less frustration. It’s all about turning daily challenges into proud accomplishments.
Physical Therapy for Core Strength and Balance
Physical Therapy (PT) is a foundational piece of the puzzle, especially when addressing the low muscle tone autism spectrum connection. Think of a physical therapist as a coach for your child’s core movements. Their main job is to build up core strength, sharpen balance, and improve those big-picture gross motor skills—the ones involving the arms, legs, and torso.
You'll find that PT sessions are designed to feel more like play than work. The activities are fun, engaging, and purposeful.
- Obstacle Courses: These are fantastic for encouraging climbing, crawling, and balancing, which naturally builds core muscles and improves motor planning.
- Balance Beam Walking: This is a fun, direct way to target and improve coordination and stability.
- Ball Activities: Sitting or bouncing on large therapy balls is a great way to "wake up" and strengthen the core muscles needed for good posture.
The goal is simple: make movement more efficient and less exhausting. This helps kids keep up on the playground and join in on the physical fun they might otherwise miss.
Occupational Therapy for Daily Living Skills
While PT is busy with the big movements, Occupational Therapy (OT) zooms in on the fine motor skills and sensory processing kids need for everyday life. An occupational therapist helps children master the "jobs" of being a kid—things like playing, learning, and taking care of themselves.
OT is the bridge between a child’s physical abilities and the practical demands of their world. It’s all about building functional skills that boost independence, from tying shoes to holding a crayon.
A typical OT session is packed with activities designed to improve:
- Hand-Eye Coordination: This could involve anything from stringing beads to putting together puzzles.
- Grasping Strength: Therapists often use therapeutic putty or squishy toys to build up those small but mighty hand muscles.
- Self-Care Routines: They’ll practice the little things that make a big difference, like buttoning a shirt, using a fork, or brushing teeth.
Speech-Language Pathology for Oral-Motor Control
Hypotonia doesn't just stop at the limbs; it can also weaken the small muscles in the face, jaw, and tongue. That’s where a Speech-Language Pathologist (SLP) becomes so important. They step in to address oral-motor control issues that can create challenges with both speaking and eating.
An SLP works to strengthen these muscles to improve articulation, making speech clearer and easier for others to understand. They are also experts in tackling feeding challenges, like trouble with chewing or swallowing, which are quite common when oral muscle tone is low.
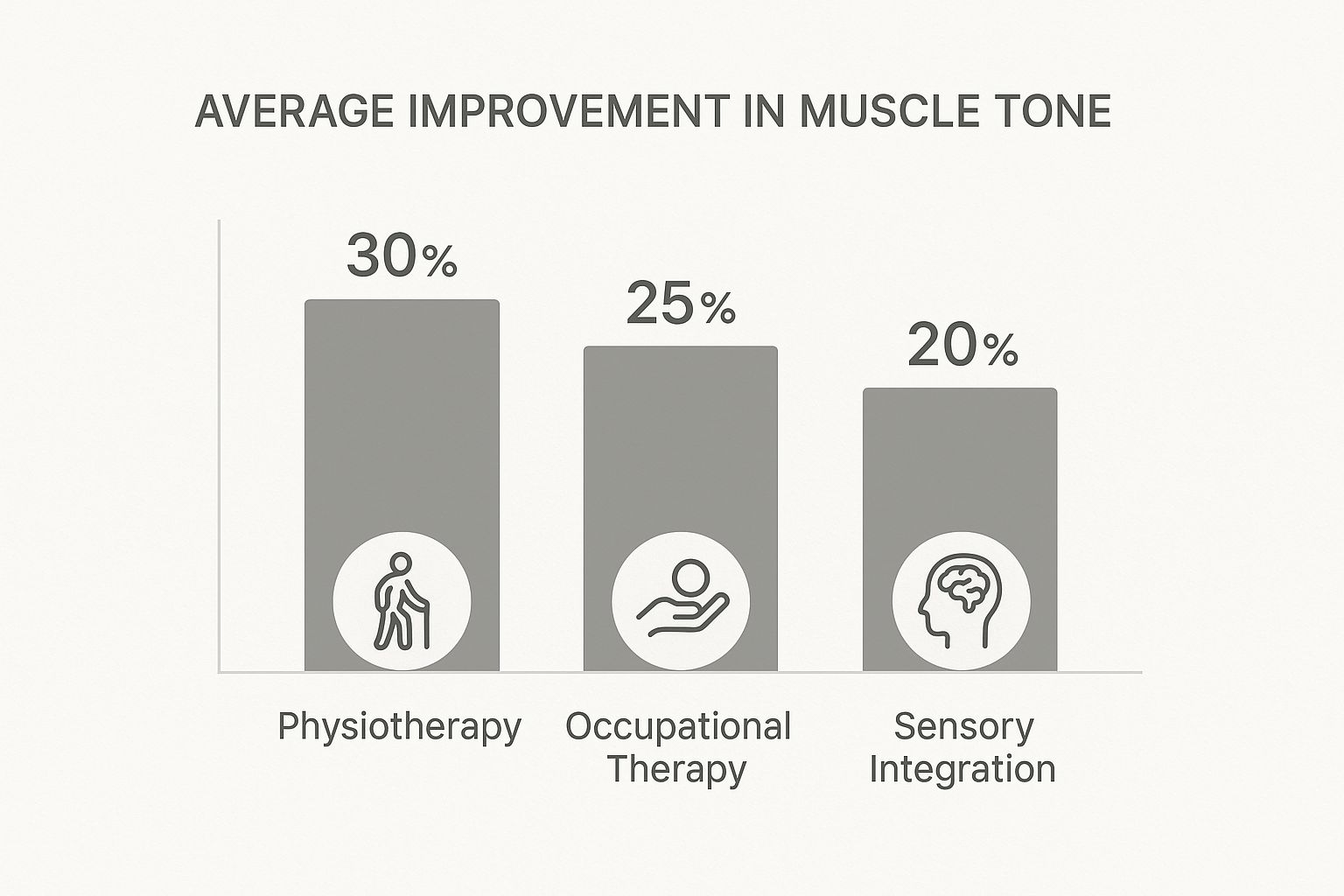
To help you see how these therapies fit together, here’s a quick comparison of their goals and methods.
Comparing Key Therapies for Hypotonia
This table breaks down the primary focus and typical activities for each therapy. Understanding these distinctions can help you and your child's care team decide on the best mix of support.
| Therapy Type | Primary Focus | Examples of Activities |
|---|---|---|
| Physical Therapy (PT) | Core strength, balance, and gross motor skills | Obstacle courses, balance beam, therapy ball exercises |
| Occupational Therapy (OT) | Fine motor skills, sensory integration, and daily self-care | Puzzles, using therapeutic putty, practicing buttoning |
| Speech-Language Pathology (SLP) | Oral-motor control, articulation, and feeding skills | Blowing bubbles, tongue exercises, chewing practice |
Each of these therapies plays a distinct yet interconnected role in supporting a child’s development. They aren’t meant to work in isolation; in fact, they’re most powerful when they work together.
As you can see, a combined approach often brings the best results. A team-based strategy ensures your child gets the well-rounded support they need to truly thrive. For families looking at care from a neurological perspective, it's also worth learning more about the connection between chiropractors and autism and how that approach can complement these foundational therapies.
How Chiropractic Care Supports Nervous System Function

Since the struggles with low muscle tone autism spectrum are tied so deeply to the nervous system, it just makes sense to look for care that focuses on this master control system. This is where neurologically-focused pediatric chiropractic steps in, offering a unique approach that works alongside traditional therapies like PT and OT.
It’s crucial to be clear on one thing: chiropractic care doesn't "treat" or "cure" autism. Instead, the goal is to optimize how the central nervous system is functioning. This system is the command center for everything—motor control, sensory processing, and even emotional regulation. By improving the communication between the brain and the body, we can create a better internal foundation for a child’s development.
Picture the nervous system as a busy highway system. When you have roadblocks or traffic jams—what chiropractors call subluxations—the messages just can't get through efficiently. For a child with low muscle tone, this might mean the brain's signals telling their muscles to stay "on" and ready are weak, garbled, or inconsistent.
Restoring Brain-Body Communication
Neurologically-focused pediatric chiropractors use incredibly gentle and precise adjustments to help clear those roadblocks. These adjustments are specifically designed to reduce interference in the nervous system, allowing for stronger, clearer communication. It’s like upgrading a bumpy country road into a smooth, multi-lane freeway.
When that communication gets better, the brain can more effectively coordinate all of the body's essential functions.
This improvement can create a positive ripple effect throughout a child's development, supporting the very systems that other therapies are working so hard to build upon.
By addressing underlying neurological stress and interference, pediatric chiropractic care helps set the stage for other therapies to be more effective. When the body's internal signaling is clearer, a child is better equipped to build strength, coordination, and new skills.
A Foundation for Better Function
The benefits of a better-functioning nervous system can show up in several key areas that are often a struggle for kids on the autism spectrum. By supporting the body’s master control system, chiropractic care aims to enhance the very tools a child uses to interact with their world.
Potential areas of improvement can include:
- Enhanced Motor Control: Clearer signals may lead to better muscle activation, improved posture, and more fluid coordination.
- Improved Sensory Processing: A calmer, more organized nervous system can better handle all the sensory information coming in from the environment.
- Better Regulation: When internal stress is reduced, it can be easier for a child to regulate their emotions and even improve sleep patterns.
This approach is all about creating a more stable neurological foundation, giving children a stronger platform from which to grow. It’s about helping their bodies work as efficiently as possible, empowering them to get the most out of every therapy session and life experience.
Common Questions About Hypotonia and Autism
When you’re navigating the world of low muscle tone and autism, it’s natural to have a lot of practical questions pop up. Getting clear, straightforward answers is a huge part of feeling confident as you support your child, so let's tackle some of the most common concerns parents bring to us.
One of the first things parents often ask is whether a child can "outgrow" hypotonia. The simple answer is no—low muscle tone isn't like a cold; it's a lifelong characteristic tied to how the nervous system is wired. But that is definitely not a reason to lose hope. Through consistent, targeted therapies like PT and OT, kids can build incredible strength, coordination, and functional skills, drastically reducing the impact hypotonia has on their day-to-day lives.
What Should I Do If I Suspect Hypotonia?
If you're noticing things like persistent slouching, frequent tumbles, or your child struggling with motor tasks that seem easier for their peers, the most important first step is to trust your instincts. Bring up your specific observations with your pediatrician. From there, you can ask for referrals to get a full picture from specialists.
The key professionals to consult usually include:
- A Pediatric Neurologist: They can help rule out other underlying causes and give a clear diagnosis.
- A Physical Therapist (PT): A PT will be your go-to for assessing gross motor skills and core strength.
- An Occupational Therapist (OT): An OT will evaluate fine motor skills, sensory processing, and daily living activities.
Getting these assessments done early is the best way to get the right support in place as soon as possible.
The goal isn’t to erase hypotonia but to build a strong foundation of support around it. By strengthening muscles and improving motor patterns, we empower children to move through their world with greater ease and confidence.
How Is Pediatric Chiropractic Different?
This is another great question we hear all the time. Many people associate chiropractic care with the kind of forceful adjustments adults get for back pain, but neurologically-focused pediatric care is a completely different world. It’s incredibly gentle, precise, and focused on improving the brain-body connection.
Instead of just addressing pain, our goal is to reduce interference in the nervous system. For a child with low muscle tone and autism, this approach helps optimize the very system that controls muscle function, coordination, and sensory processing. It’s not about "cracking" anything; it's about restoring balance so the nervous system can do its job better. This creates a stronger foundation for development and can even make other therapies more effective.
At First Steps Chiropractic, we specialize in this gentle, neurologically-focused approach to help your child thrive. To see if our care is the right fit for your family, learn more at https://firststepschiropractic.com.

