Sensory Processing Disorder (SPD) is a neurological condition that makes it tough for the brain to properly receive and respond to information coming in from the senses. Think of the brain as an air traffic controller for sensory information. For a child with SPD, that controller gets completely overwhelmed, leading to sensory traffic jams that cause behaviors that can seem confusing from the outside.
It’s crucial to understand this is a real neurological challenge, not a behavioral choice.
Demystifying Sensory Processing Disorder
Imagine you're trying to have a simple conversation, but the TV is blaring, the lights are flickering, and someone is constantly tapping your shoulder. You’d probably feel overwhelmed, irritable, and completely unable to focus.
This is what everyday life can feel like for a child with SPD. Their brain misinterprets common sights, sounds, and touches, turning the gentle hum of a refrigerator into a deafening roar or the seam on a sock into something that feels painfully irritating.

This is why Sensory Processing Disorder is so much more than just being a "picky eater" or "overly sensitive." It’s about the brain's fundamental ability to organize all the sensory input it receives just to get through the day.
A Neurological Perspective
The concept of sensory integration isn't new; it was first developed by occupational therapist Anna Jean Ayres way back in the 1960s. Today, we understand Sensory Processing Disorder as a condition where the brain really struggles to receive, organize, and respond to sensory input in an appropriate way. This can impact everything from a child's balance and motor skills to their emotional regulation and ability to make friends.
To provide a quick reference, here’s a simple breakdown of what SPD involves:
Key Aspects of Sensory Processing Disorder at a Glance
| Component | Simple Explanation | Common Impact |
|---|---|---|
| Sensory Input | Information received through the senses (touch, sound, sight, taste, smell, movement, body awareness). | A child might be overly sensitive (hyper-responsive) or under-sensitive (hypo-responsive) to things like noise, light, or textures. |
| Neurological Processing | The brain’s job of organizing and making sense of this sensory information. | The brain struggles to filter what's important, leading to feelings of being overwhelmed or "stuck." |
| Behavioral Response | The actions and emotions that result from how the brain processes sensory input. | This can look like meltdowns, avoiding certain activities, seeking intense sensory input (crashing, spinning), or social withdrawal. |
This table helps show that SPD isn't just one thing; it's a complex interplay between what a child senses, how their brain handles it, and how they ultimately react.
At its core, SPD is a breakdown in how the nervous system manages all the sensory messages it’s constantly receiving. The brain either overreacts, underreacts, or desperately seeks out intense sensations just to make sense of the world around it.
Understanding this neurological basis is the first step toward true empathy and effective support. Instead of seeing a "difficult" child, we can start to see a child whose brain is working overtime just to navigate a world that feels chaotic and unpredictable.
This shift in perspective is everything. It moves the focus from simply managing behavior to addressing the underlying sensory needs that are driving it. For parents exploring how different therapies can support the nervous system, you might find our guide on pediatric chiropractic for sensory disorders helpful. This approach helps reframe the challenges into opportunities for targeted, compassionate intervention.
Recognizing the Signs of Sensory Processing Disorder
Every child has their own little quirks, but when certain sensitivities and behaviors start to form a consistent pattern, it might be a sign that their brain is wired to interpret the world a little differently. Recognizing the signs of Sensory Processing Disorder isn't about slapping a label on every fussy moment. It’s about understanding the "why" behind your child's reactions.
When you start to see their actions through a sensory lens, things can suddenly click into place.
These challenges are a lot more common than most people think. Research shows that SPD affects somewhere between 5% and 16.5% of school-aged children. To put that in perspective, in a kindergarten class of 30 kids, at least one or two (and maybe more) could be navigating these sensory difficulties every single day. You can explore the full research on SPD prevalence here.
The signs of SPD usually fall into three main categories, though it’s very common for a child to show a mix of traits across their different senses.
Sensory Over-Responsivity: The Avoider
For some kids, the world feels like it's turned up to full volume all the time. This is sensory over-responsivity, where ordinary, everyday input feels intense, overwhelming, or even painful. These children often become "avoiders," doing everything they can to escape sensations that cause them genuine distress.
You might be seeing this pattern if your child:
- Has extreme reactions to sudden or loud noises like a vacuum cleaner, a public bathroom hand dryer, or a blender.
- Is an extremely picky eater, refusing foods based on their texture, smell, or even the way they look on the plate.
- Can't stand certain clothes, complaining that tags are unbearably itchy, seams are painful, or that a perfectly normal fabric feels "scratchy."
- Avoids messy play at all costs—no finger painting, no sandboxes, and definitely no walking barefoot on the grass.
A child who is over-responsive might have a massive meltdown in a crowded grocery store. It's not because they're being defiant, but because the combination of bright fluorescent lights, humming freezers, and dozens of conversations is a true sensory assault on their nervous system.
Sensory Under-Responsivity: The Unaware Child
On the flip side of the coin is sensory under-responsivity. For these children, it's as if the world is muted. Their nervous system needs a much stronger signal to register what's going on, which can often make them seem passive, withdrawn, or "in their own world."
Signs of under-responsivity might include:
- Appearing oblivious to what's happening around them, often not responding when their name is called.
- Having a surprisingly high pain tolerance, sometimes not even noticing scrapes or bruises.
- Seeming clumsy, uncoordinated, or having poor body awareness.
- Showing little or no reaction to intense sensations like extreme cold or heat.
Sensory Craving: The Seeker
The third pattern is sensory craving, which is exactly what it sounds like. These kids are on a constant mission for more—more input, more intensity, more everything. Their nervous system is actively seeking out strong sensory experiences just to feel organized and regulated. These are the "seekers," the kids who seem to be in constant motion.
A sensory craver might:
- Need to touch everything and everyone, sometimes not realizing they're in someone else's personal space.
- Love crashing, jumping, and roughhousing, often with more force than they intend.
- Fidget constantly, chew on their shirt collar or other non-food items, and find it almost impossible to sit still.
- Crave intense movement like spinning in circles, swinging as high as possible, or being tossed in the air.
Understanding which of these patterns fits your child is the first, most important step. It helps you shift your perspective from asking, "Why won't my child behave?" to wondering, "What is my child's nervous system trying to tell me?" This simple change in perspective is incredibly empowering and opens the door to finding real, effective ways to help them feel more comfortable in their world.
Understanding the Causes and Risk Factors
When you first get a diagnosis of Sensory Processing Disorder, one of the first questions that bubbles to the surface is, "Why? Why my child?" It's a completely natural question, and it often comes with a heavy dose of guilt or worry.
Let’s get one thing straight right away: SPD is not caused by something you did or didn't do.
This condition is complex, and we can’t point to a single, simple cause. What we do know is that it’s all about how a child's nervous system gets wired during development. Think of it less like a mistake in parenting and more like a unique blueprint for their neurology.
It’s like baking a cake from a very complex recipe. A child’s unique sensory profile is shaped by a mix of genetic ingredients they inherit and a whole host of environmental factors they experience, starting from before they were even born.
Genetic and Environmental Influences
Research is increasingly showing us that sensory processing challenges can run in families. If a parent or another close relative has sensory quirks or sensitivities, it’s not surprising that a child might have them, too. But that’s only one piece of the puzzle.
Environmental factors, especially things that happen during those critical windows of development, also play a huge role. Studies have started to connect the dots between certain prenatal and birth experiences and a higher likelihood of a child developing sensory challenges later on.
It's so important to remember that these are just correlations, not direct causes. Plenty of kids experience these risk factors and develop perfectly typical sensory systems. On the flip side, some kids with no known risk factors end up with significant sensory challenges.
These factors are simply part of your child’s unique story. Research has found that things like a low birth weight (under 2200 grams), premature birth (before 36 weeks), and major complications during pregnancy can increase the odds. Even things like significant maternal stress or illness during pregnancy are thought to be part of that complex recipe. You can discover more insights about these research findings on SensoryHealth.org.
Ultimately, learning about these potential influences isn't about placing blame. It’s about understanding the incredible, intricate journey your child’s nervous system has been on from day one. This knowledge helps us shift our focus from "what went wrong?" to "what does my child need now?"—allowing us to provide compassionate, proactive support that truly fits their needs.
Navigating the Diagnostic Journey
If you're starting to suspect your child might have a sensory processing disorder, the idea of getting a diagnosis can feel pretty overwhelming. Where do you even begin? The good news is that the path to getting clear answers is more straightforward than you might think, and it all starts with finding the right professional to guide you.
Your main expert on this journey will likely be an occupational therapist (OT), especially one with specialized training in sensory integration. OTs have a unique gift for looking at the whole child—how they play, how they interact, and how they handle daily tasks—to truly understand what’s going on inside their sensory system. They don’t just see the behaviors on the surface; they dig deeper to find the sensory reasons behind them.
Getting to the bottom of it isn't a quick checklist or a simple medical test. A proper, thorough assessment is really a deep dive into your child’s unique sensory world.
What to Expect During an Evaluation
A comprehensive evaluation is all about painting a complete picture of your child. It typically involves a few key parts to make sure the final recommendations are a perfect fit for your child's specific needs and struggles.
The process usually includes:
- Standardized Testing: This involves specific, research-backed activities that compare your child's sensory processing abilities to other kids their age. It gives the OT a solid baseline.
- Structured Observations: This is where the fun comes in! The OT will engage your child in specific play-based activities, carefully watching how they react to different sensory inputs and motor challenges in a controlled, comfortable setting.
- Parent Interviews: This is one of the most critical pieces of the puzzle. You are the expert on your child. The OT will ask you detailed questions about their developmental history, daily routines, and the specific behaviors you’ve been seeing at home and in school.
The whole point of an evaluation isn't just to get a label. It's to create a detailed "sensory map" of your child. This map shows their strengths, their sensitivities, and the exact areas where their nervous system needs more support to really thrive.
From Assessment to Action Plan
After the evaluation, the OT will pull together all the information—from the tests, the observations, and your own expert insights. This all comes together in a detailed report that clearly outlines your child’s specific sensory patterns and provides clear, actionable recommendations.
This report becomes the foundation of your child's therapy plan. It turns the confusion of "what is sensory processing disorder?" into a clear roadmap for support, both in therapy sessions and at home. For more foundational knowledge, you can also explore our detailed overview of sensory processing disorder.
Armed with this comprehensive assessment, you can step into your role as a confident advocate, fully equipped to help your child navigate their world with far more ease and success.
Exploring Effective Therapies and Treatments
Once you have a better handle on your child's unique sensory needs, the focus shifts from just identifying the challenges to finding real, effective solutions. This is the moment where hope turns into action. A diagnosis of sensory processing disorder isn’t a label; it’s a key that unlocks targeted therapies designed to help your child’s brain build stronger, more efficient pathways for managing sensory information.
The cornerstone of SPD treatment is Occupational Therapy (OT), especially when it’s grounded in a Sensory Integration (OT-SI) approach. Forget what you might picture when you hear "therapy." To your child, it will feel a lot more like structured, intentional play.
Occupational Therapy with a Sensory Integration Focus
An OT session often unfolds in a "sensory gym" — a space filled with specialized equipment like swings, therapy balls, crash pads, and bins full of different textures. The occupational therapist’s goal is to present your child with the "just right" challenge. These are activities that are fun and engaging but also gently push their nervous system to adapt and forge new connections.
These playful activities all serve a profound neurological purpose:
- Swinging helps the vestibular system better process movement and improve balance.
- Climbing provides deep proprioceptive input, which enhances body awareness and motor planning.
- Playing in a tactile bin with materials like sand or beans can help desensitize a child who is sensitive to certain textures.
The core idea behind OT-SI is that through these carefully chosen sensory experiences, the brain can actually learn to process information more effectively. It’s like paving a bumpy, winding dirt road into a smooth, direct highway, allowing sensory traffic to flow much more freely.
This approach is never one-size-fits-all. The therapist uses their deep understanding of your child's sensory profile to craft activities that meet their specific needs, whether they are sensory-avoiding, under-responsive, or sensory-seeking.
The Power of a Multi-Faceted Approach
While OT is often the primary intervention, a truly successful plan usually brings in a variety of supportive strategies. Think of it like building a house: OT lays the foundation, but other therapies and tools add the walls, roof, and supports that make the whole structure strong and secure.
Supportive therapies might include speech therapy to address oral motor sensitivities or physical therapy to improve posture and coordination. Another crucial piece is creating a "sensory diet" at home. This is a personalized schedule of sensory activities designed to keep your child’s nervous system regulated and balanced throughout the day.
This chart visualizes the reported improvement rates for several key SPD interventions.
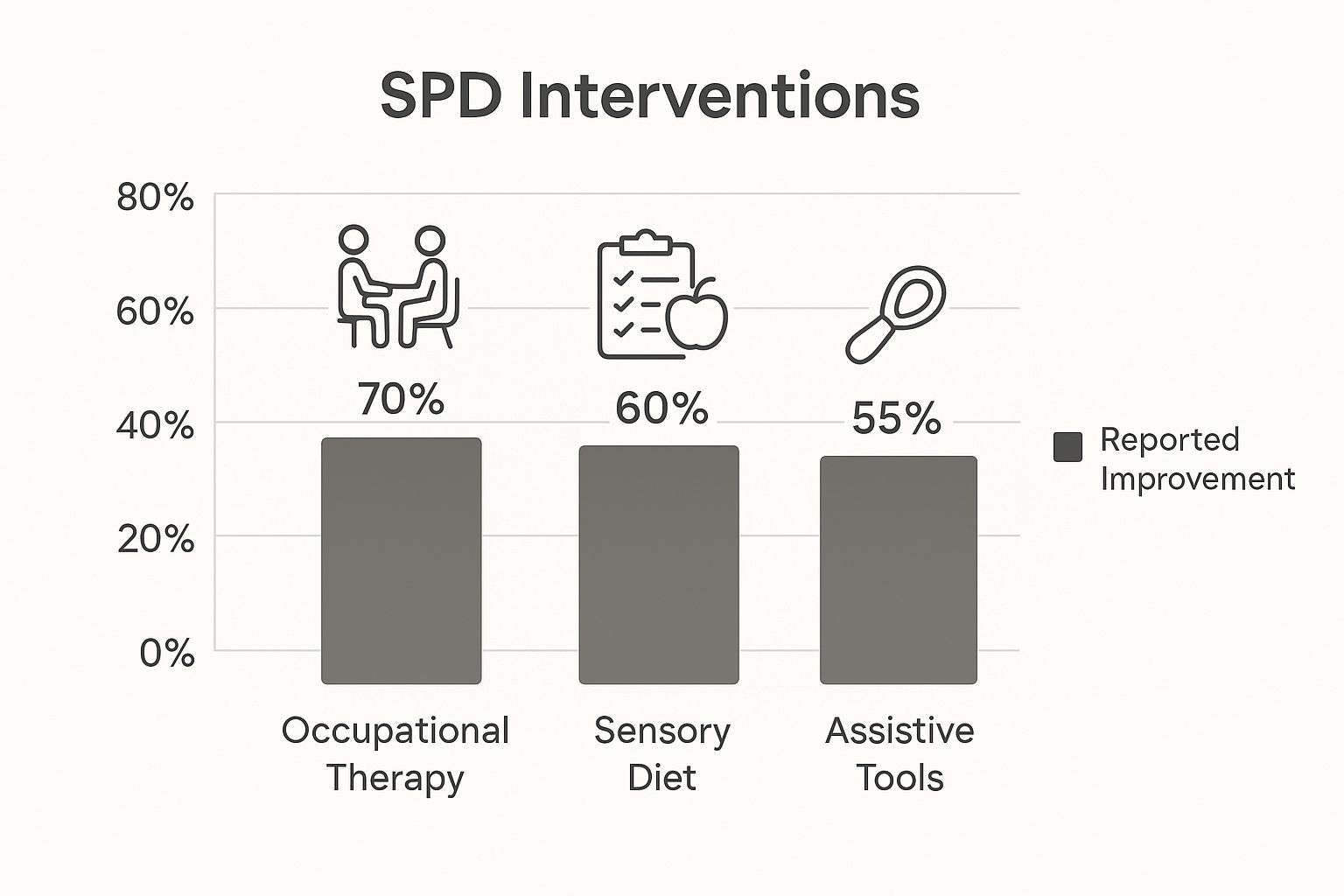
As the data shows, combining professional therapy with consistent at-home strategies creates a powerful support system for a child with SPD.
Comparing Therapeutic Approaches for SPD
To help you understand the landscape of SPD support, this table breaks down the most common interventions, showing how they differ in their focus and goals.
| Therapy Type | Core Focus | Example Activities | Primary Goal |
|---|---|---|---|
| Occupational Therapy (OT-SI) | Improving the brain's ability to process and organize sensory input through structured play. | Swinging, jumping on a trampoline, playing in tactile bins, obstacle courses. | Enhance sensory integration, improve motor skills, and support self-regulation. |
| Physical Therapy (PT) | Strengthening gross motor skills, improving posture, balance, and coordination. | Balance beam walking, core strengthening exercises, ball skills. | Improve body awareness, motor control, and functional movement. |
| Speech-Language Therapy | Addressing feeding issues, oral motor sensitivities, and communication challenges. | Blowing bubbles, chewing on resistive toys, practicing social communication. | Improve feeding skills, reduce oral defensiveness, and enhance social interaction. |
| Neuro-Tonal Chiropractic | Optimizing nervous system function by addressing spinal misalignments (subluxations). | Gentle, specific adjustments to the spine. | Regulate the nervous system, reduce stress, and improve brain-body communication. |
Each of these therapies offers a unique piece of the puzzle. When they work in concert, they create a comprehensive network of support that helps your child feel more comfortable and confident in their own skin.
For a deeper dive into how different approaches can be combined, our guide on sensory processing disorder therapy offers additional insights. Ultimately, the goal isn't to "fix" your child, but to empower them with the tools and skills they need to thrive in a world that can often feel overwhelming.
Everyday Strategies to Support Your Child at Home
As a parent, you are your child’s anchor. While professional therapies are an essential part of the plan, the small, consistent changes you make right at home can create the most profound and lasting impact. Creating a sensory-friendly environment isn’t about a massive home makeover; it’s about making thoughtful, intentional adjustments that help regulate your child’s nervous system all day long.
One of the best tools you have for this is a sensory diet. No, it has nothing to do with food! Think of it as a personalized schedule of activities, specifically designed to give your child the right kind of sensory input they need to feel calm, focused, and organized. Just like a balanced diet nourishes the body, a sensory diet nourishes the brain and nervous system.
Building a Personalized Sensory Diet
A sensory diet is all about being proactive, not reactive. The idea is to weave sensory input into your child's day before their system gets overwhelmed or under-stimulated, which is often what leads to those tough meltdowns or moments of dysregulation. While an occupational therapist is your best partner for creating a detailed plan, you can absolutely start with some simple, powerful strategies right away.
The key is to think about activities that match your child’s specific sensory profile.
- For the Sensory Seeker: You’ll want to incorporate activities that give them that big, intense input they crave. This helps them feel grounded and organized without having to resort to crashing into the couch.
- For the Sensory Avoider: The focus here is on calming, predictable activities. These help lower their state of arousal and create a feeling of safety and security.
- For the Under-Responsive Child: Look for activities that help "wake up" their system and increase their awareness of their body and their surroundings.
When you start weaving these activities into your daily routine, you help your child maintain a state of balance. This makes it so much easier for them to handle all the natural ups and downs of life.
Practical Ideas for Your Home Environment
Making your home a true sensory haven involves two things: adding supportive elements and removing overwhelming ones. You'd be amazed at how a few small tweaks can make a world of difference in your child's comfort, happiness, and ability to cope.
Creating Calming Spaces for Over-Responders:
If your child gets easily overwhelmed by noise, bright lights, or too much action, a designated quiet space can be a total lifesaver. This isn't a "timeout" spot—it's a safe retreat they can choose to go to when they feel their sensory engine revving up too high.
Think of it as their personal "sensory reset button." A cozy corner with soft pillows, a weighted blanket, noise-canceling headphones, and a few favorite calming fidgets can give their nervous system the break it needs to recalibrate before stress boils over into a meltdown.
Incorporating 'Heavy Work' for Sensory Seekers:
Kids who constantly crave intense physical input get so much out of heavy work. These are simply tasks that involve pushing, pulling, or carrying things, which provides deep, calming pressure to the muscles and joints. This kind of input has an incredibly powerful organizing effect on the brain.
It’s surprisingly easy to build this into everyday chores:
- Carrying the laundry basket to the laundry room.
- Pushing the vacuum cleaner (even a toy one works!).
- Helping bring in groceries from the car.
- Watering plants with a small watering can.
These simple jobs give their bodies the intense feedback they're looking for in a productive, structured way. This often reduces their need to seek it out by jumping on furniture or wrestling a little too roughly. By understanding what sensory processing disorder is and seeing how it shows up in your child, you can turn everyday routines into powerful therapeutic opportunities, empowering them to feel more in control and at peace in their own world.
At First Steps Chiropractic, we specialize in helping children's nervous systems function at their absolute best. Our gentle, neurologically-focused approach can be a powerful and effective addition to your child's support plan. Schedule a complimentary consultation today to learn how we can help your family thrive.

