Silent reflux symptoms can be tricky. They often show up as a chronic cough, constant throat clearing, or hoarseness instead of the classic, fiery heartburn associated with GERD. This condition, officially known as Laryngopharyngeal Reflux (LPR), happens when stomach contents travel all the way up to the delicate tissues of your throat and voice box.
Unmasking The Elusive Nature Of Silent Reflux
Have you ever been stuck with a nagging cough that just won’t quit? Or maybe you have that persistent feeling of a lump in your throat. While it’s easy to blame allergies or a cold that’s overstaying its welcome, the real culprit could be silent reflux.
Unlike its more famous cousin, Gastroesophageal Reflux Disease (GERD), LPR often flies completely under the radar because it doesn't usually cause that tell-tale heartburn. This is the biggest challenge for families—spotting a problem whose signs are subtle and so easily mistaken for something else.
A Mist Versus a Wave
To really get the difference, picture GERD as a powerful wave of acid splashing up from the stomach into the esophagus. You feel that burn almost immediately.
Now, think of silent reflux as a persistent, irritating mist. This isn’t just acid; it's a mix of stomach contents, including digestive enzymes like pepsin, that rises much higher. It settles in the throat, the voice box, and sometimes even the nasal passages.
This fine mist doesn’t always cause a burning feeling, but over time, its effect on these delicate tissues—which aren't built to handle it—leads to inflammation and a whole different set of symptoms. The diagram below really helps visualize how the pathways differ.
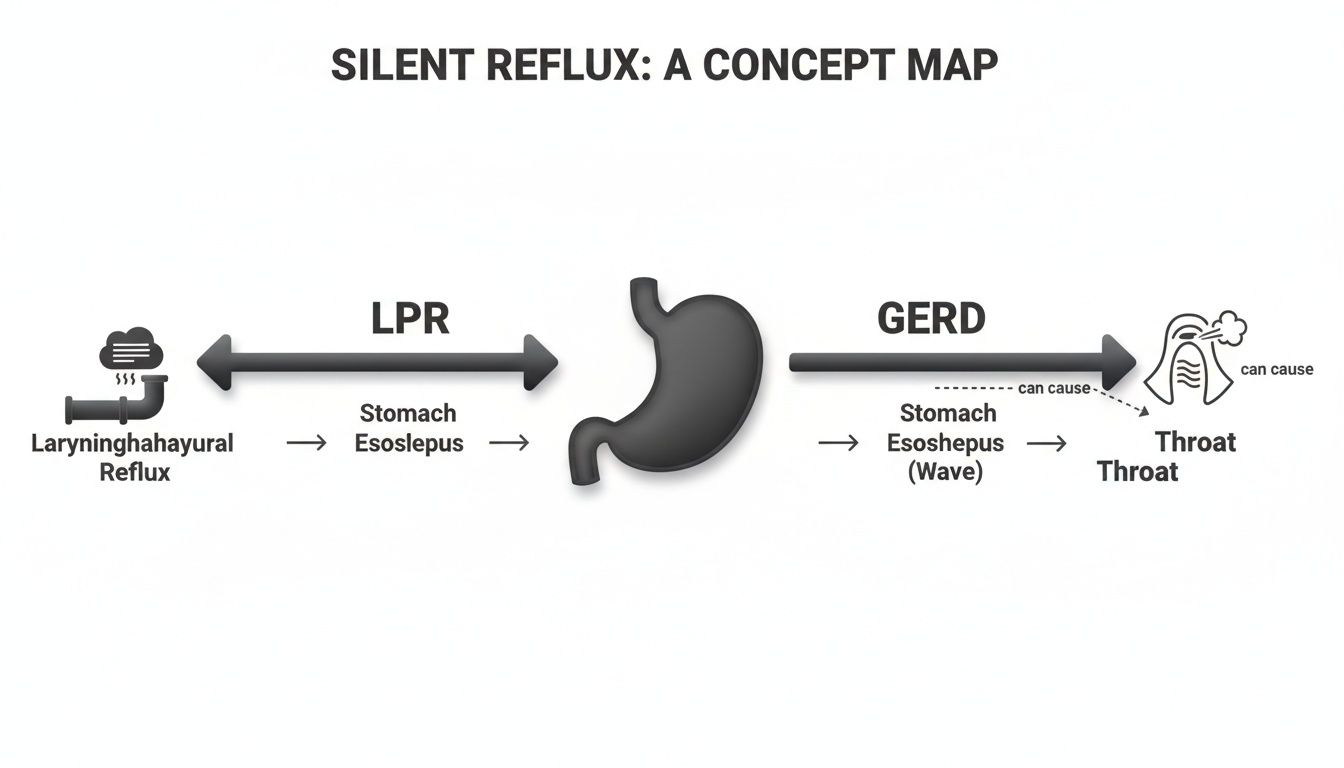
As you can see, LPR's impact is focused on the throat and larynx, while GERD primarily affects the lower esophagus.
How Common Is Truly Silent Reflux?
That "silent" part isn't just a catchy name; it's a clinical reality. Many people experience significant internal irritation without feeling any obvious discomfort.
Research has shown that a surprising number of patients with proven esophageal damage from reflux report no symptoms at all. In fact, some studies found this was true for up to 36.8% of individuals with erosive esophagitis. You can dig into more of the research on reflux without heartburn to see just how common it is.
Since the symptoms are so deceptive, understanding the key differences between LPR and GERD is the first real step toward getting the right answers and support for your family. This table breaks down the main distinctions to help you start connecting the dots.
Silent Reflux (LPR) vs Classic Reflux (GERD) At a Glance
Here’s a quick comparison to help you differentiate between the two conditions based on their common symptoms and what’s happening inside the body.
| Feature | Silent Reflux (LPR) | Classic Reflux (GERD) |
|---|---|---|
| Primary Symptom | Chronic cough, hoarseness, throat clearing, feeling of a lump in the throat. | Heartburn, chest pain, acid regurgitation. |
| Symptom Timing | Often worse during the day, especially after meals, when upright. | Typically worse at night or when lying down. |
| Substance Refluxed | A fine mist of stomach contents, including acid and enzymes (pepsin). | Liquid stomach acid. |
| Affected Area | Larynx (voice box), pharynx (throat), and upper airway. | Esophagus (the tube connecting the throat and stomach). |
| Common Complaint | "I constantly have to clear my throat." | "I have a burning pain in my chest." |
Recognizing which set of symptoms aligns with your experience is crucial, as it guides the conversation with your healthcare provider and points toward the most effective management strategies.
Decoding Silent Reflux Symptoms in Infants and Children
As a parent, there’s nothing harder than seeing your little one uncomfortable and not knowing why. Silent reflux can be especially tricky because the clues are often subtle and easily dismissed as normal baby fussiness. Unlike the dramatic spit-up we associate with classic reflux, the symptoms of silent reflux are much quieter—but they are just as disruptive to your child’s well-being.
Learning to spot these signs is the first real step toward finding gentle, effective support. Since babies can't tell you what's wrong, parents have to become detectives, piecing together a puzzle from small, seemingly unrelated behaviors. For so many families, finally understanding the root cause brings an immense sense of relief and empowerment.

Uncovering Infant Reflux Clues
In infants, the signs of silent reflux often pop up around feeding and sleep, turning what should be peaceful moments into stressful ones. Instead of projectile vomiting, you’re looking for less obvious signs of distress that happen when stomach contents travel up and irritate their delicate throat.
Here are some of the most common silent reflux symptoms in babies:
- Arching the Back During or After Feeds: This is a classic sign of pain. Your baby might suddenly stiffen their body and arch away from the breast or bottle, almost as if they're trying to escape the discomfort.
- Frequent "Wet" Burps or Hiccups: These aren't just cute baby sounds. If a burp sounds wet or the hiccups are constant and gurgly, it can mean a small amount of stomach acid is coming up with the air.
- Chronic Nasal Congestion or Stuffiness: Does your baby always seem stuffy but never actually has a cold? This could be from refluxed contents irritating their nasal passages and causing inflammation.
- Disrupted and Restless Sleep: Babies with silent reflux often hate sleeping flat on their backs. They might grunt, squirm all night, or wake up frequently in discomfort because lying horizontally can make the reflux worse.
- A Hoarse or Gurgly-Sounding Cry: Persistent irritation of the vocal cords from acid can lead to a hoarse-sounding cry. You might also hear a gurgling in their chest or throat, especially when they’re lying down.
These signs can be incredibly frustrating for parents, often leading to feelings of helplessness. It's important to remember that this discomfort is often linked to underlying nervous system dysregulation, where the body's "rest and digest" system isn't functioning optimally.
Understanding these signals helps shift the focus from just managing symptoms to addressing the root cause. While these behaviors can be perplexing, it's also important to distinguish them from other common infant issues. For more insights, you can explore the key differences between colic versus reflux in our detailed guide.
Identifying Symptoms in Toddlers and Older Children
As children get older, the symptoms of silent reflux can change. They become even easier to mistake for other things, like seasonal allergies or even just bad habits. Your child probably won't complain of "heartburn," but their body is still sending out signals that something isn't right.
These symptoms often show up as chronic ear, nose, and throat issues, all because that irritating mist of stomach contents keeps affecting their upper airways. Pay close attention if you notice a consistent pattern of these behaviors.
Checklist for Children and Toddlers
- Constant Throat-Clearing: Does your child have a persistent habit of clearing their throat, almost like a nervous tic? This is often an unconscious attempt to clear the mucus or irritation caused by reflux.
- Unexplained Hoarseness: A raspy or strained voice that isn't connected to a cold or a day of yelling, especially in the morning, can be a strong indicator of laryngeal irritation.
- Difficulty Swallowing (Dysphagia): You might hear your child complain that food "gets stuck." Or maybe you've noticed them taking a very long time to eat, chewing excessively, or avoiding certain textures like bread and meat.
- Feeling of a "Lump in the Throat": Known as globus sensation, this is a common complaint where a child feels like something is stuck in their throat even when there isn't. It's a direct result of inflammation in the pharynx.
- Recurring Ear or Sinus Infections: When reflux reaches the back of the throat, it can inflame the area around the Eustachian tubes, leading to fluid buildup and one ear infection after another. It can irritate the sinuses in the same way, contributing to chronic sinus problems.
Recognizing these quiet symptoms is a critical step for families searching for answers. By connecting these subtle signs to a potential underlying cause, you can begin to explore supportive strategies that focus on restoring balance to the nervous system and improving digestive function for lasting relief.
How to Recognize Silent Reflux Symptoms as an Adult
For adults, the signs of Laryngopharyngeal Reflux (LPR), or silent reflux, are masters of disguise. It’s so easy to blame the persistent symptoms on seasonal allergies, a cold you just can’t kick, post-nasal drip, or even just getting older. The real challenge is connecting all the dots between these seemingly unrelated issues and seeing them for what they are: potential silent reflux symptoms.
Unlike the fiery, unmistakable heartburn of classic GERD, LPR’s effects are much sneakier. It’s caused by a fine mist of stomach contents—acid and digestive enzymes like pepsin—traveling way up into the throat and voice box. The tissues there are incredibly sensitive and just aren't built to handle that kind of exposure, which leads to chronic inflammation and a whole host of confusing symptoms.

Connecting the Dots: A Checklist for Adults
Countless adults live with these symptoms for years without ever getting a proper diagnosis. If you’ve been struggling with any of the following, silent reflux might just be the underlying cause you've been looking for.
- Persistent Morning Hoarseness: Waking up with a gravelly, raspy voice that seems to get better as the day goes on is a classic sign. This happens because reflux is often worse when you're lying down, allowing irritants to pool around your vocal cords all night.
- A Chronic, Dry Cough: This isn't the productive, chesty cough you get with a cold. It’s a nagging, dry, and often tickly cough that comes out of nowhere, usually getting worse after you eat or lie down.
- Excessive Throat Clearing: Do you feel like you always need to clear your throat, as if something is stuck back there? That's a natural reflex to the irritation and extra mucus your body produces to protect the throat lining from reflux.
- The Feeling of a Lump in Your Throat: Medically, this is called "globus sensation." It’s that frustrating feeling that something is stuck in your throat when nothing is actually there. It’s a direct result of inflammation and muscle tension in the throat caused by reflux.
- Difficulty Swallowing (Dysphagia): Maybe you’ve noticed that pills are harder to get down, or that certain foods like bread or meat feel like they're "sticking" on the way down. This can be caused by swelling and irritation in your esophagus and throat.
The most crucial takeaway for adults is this: the absence of heartburn does not rule out reflux. In fact, this lack of a classic symptom is precisely why LPR is so frequently missed, leaving people searching for answers while the root issue goes unaddressed.
Why It Happens and How Prevalent It Is
All these different symptoms stem from the same root cause: damage to the delicate tissues of the larynx (voice box) and pharynx (throat). When the muscular valves, or sphincters, that act as gateways between the stomach and esophagus aren't working properly, stomach contents can travel much higher than they should.
And this problem is far more common than most people think. Globally, LPR affects anywhere from 5% to 30% of the population and is behind up to 10% of all visits to ear, nose, and throat (ENT) clinics. One detailed study found LPR in 31.2% of its participants, noting it was more common in women and adults between 36 and 45. These numbers show just how many adults are likely dealing with silent reflux without even knowing it. You can learn more about the prevalence and impact of laryngopharyngeal reflux.
Understanding that these chronic annoyances might be linked back to your digestive and nervous system function is the first real step toward finding relief. Instead of just treating the cough or hoarseness, a holistic approach aims to support the body’s underlying regulation to get to the true cause of the problem.
Exploring the Root Causes of Silent Reflux
To get to the bottom of the frustrating and often confusing signs of silent reflux, we need to look past the throat and dig into the actual mechanics of digestion. While the symptoms—that nagging cough or constant throat clearing—show up high, the real problem often starts with two critical "gateways" in your digestive tract and the complex nerve system that's supposed to be running the show.
Think of your digestive system as a finely tuned one-way street. Where your esophagus meets your stomach, you have the lower esophageal sphincter (LES). Up top, just below your throat, is the upper esophageal sphincter (UES). These are muscular rings, and their job is simple: open just long enough for food to pass through, then clamp shut tight to keep stomach contents exactly where they belong.
With silent reflux, or LPR, these gateways just aren't coordinating properly. It’s not usually a complete failure, but more of a subtle breakdown—a momentary relaxation at the wrong time or just poor communication between the two. This slip-up allows a fine mist of stomach acid and digestive enzymes like pepsin to sneak past both sphincters, traveling all the way up to irritate the delicate tissues in your voice box (larynx) and throat (pharynx).
Common Triggers and Risk Factors
So, what causes this breakdown in the first place? Several physiological and lifestyle factors can make it harder for these gateways to do their job, essentially weakening their resolve. Pinpointing these can be a huge first step toward getting things back on track.
Here are some of the most common culprits:
- Dietary Choices: Highly acidic, spicy, or fatty foods can be major triggers. Things like caffeine, chocolate, and fizzy drinks can either ramp up stomach acid production or directly cause the LES to relax when it shouldn't.
- Obesity: Extra weight, especially around the abdomen, puts constant physical pressure on the stomach. This pressure can literally force stomach contents upward, overpowering the LES.
- Chronic Stress: Stress isn't just in your head; it has a direct, physical impact on your body. It kicks your system into a "fight or flight" mode, which can throw your entire digestive process, including the function of these sphincters, into chaos.
- Hiatal Hernia: This is a structural issue where part of the stomach pushes up through the diaphragm. This physically weakens the LES and makes reflux far more likely to occur.
The rise of these risk factors is becoming a major health concern. Globally, the burden of reflux-related conditions has skyrocketed, with cases jumping by a staggering 83.2% between 1990 and 2021. And the trend is expected to continue, which really highlights the need for better ways to manage it. You can explore the full research on rising GERD prevalence to get a sense of the scale of this issue.
The Master Controller: The Vagus Nerve
While lifestyle factors are a big piece of the puzzle, there’s often a deeper layer at play: the nervous system. The entire digestive symphony—from swallowing to sphincter control to the speed at which your stomach empties—is conducted by one master controller: the vagus nerve.
The vagus nerve is the main communication highway between your brain and your digestive system. It's what tells the sphincters when to open and close, regulates acid production, and makes sure food moves smoothly through your gut.
When the signals from this nerve get scrambled or interfered with, the whole system can fall out of sync. Imagine a traffic controller giving confusing signals at a busy intersection—chaos ensues. The gateways might open when they should be closed, or their clamping pressure might be too weak to hold back reflux. This neurological interference can be a primary root cause of conditions like LPR, which helps explain why symptoms often stick around even after someone has perfected their diet.
This brain-gut connection is especially vital for infants and children, whose nervous systems are still maturing. Things like stress during pregnancy, a difficult birth, or other early life challenges can create interference in these critical nerve pathways.
For long-term relief, we have to restore clear communication along this nerve. By focusing on optimizing the function of the nervous system, we can help the body regain proper control over its digestive gateways. This approach allows us to address the root of silent reflux instead of just chasing its elusive symptoms. You can learn more about vagus nerve function in our detailed article and see how deeply it’s connected to overall wellness.
A Gentle Path to Relief and Supportive Strategies
Understanding the potential causes and recognizing the elusive signs of silent reflux is a huge step forward. Now, we can shift our focus toward empowering you with practical, actionable steps to find relief. This isn't about a single quick fix but a supportive plan that combines well-established advice with gentle, family-centered strategies to restore balance.
Managing silent reflux symptoms effectively almost always involves a multi-faceted approach. By addressing diet, lifestyle, stress, and underlying neurological function, families can create a solid foundation for lasting comfort and well-being. The goal is to calm the entire system, reduce irritation, and support the body’s natural ability to regulate itself.
Lifestyle and Dietary Adjustments
Sometimes the simplest changes to daily routines and eating habits can make a significant difference in reducing the frequency and severity of reflux episodes. Think of these adjustments as the foundation of your plan, working to minimize the triggers that can lead to discomfort for both kids and adults.
You're essentially creating a calmer internal environment where the digestive system isn’t constantly under pressure. These strategies are often the first line of defense and can provide substantial relief on their own.
A few key adjustments include:
- Smaller, More Frequent Meals: Big meals stretch the stomach and increase pressure on the lower esophageal sphincter (LES)—that critical gateway. Offering smaller portions more often keeps the stomach from getting overly full and pushing contents back up.
- Avoiding Trigger Foods: We all have them. Common culprits for reflux include acidic foods like tomatoes and citrus, spicy dishes, fatty or fried foods, chocolate, and carbonated drinks. Keeping a simple food journal for a week or two can be incredibly revealing and help you pinpoint specific triggers for you or your child.
- Timing is Everything: Try to avoid eating for at least three to four hours before lying down for bed. This gives the stomach plenty of time to empty, using gravity to your advantage to keep everything settled.
- Elevate the Head of the Bed: For adults and older children, raising the head of the bed by six to eight inches can work wonders. For infants, always, always follow safe sleep guidelines and consult your pediatrician before making any adjustments to their sleep space.
The Critical Role of Stress Management
The connection between stress and digestive issues is profound and well-documented. When the body is stressed, it flips on the "fight or flight" response, diverting energy away from functions it deems non-essential in that moment—like digestion. This can mess with the coordination of the esophageal sphincters and slow down stomach emptying, creating the perfect storm for reflux.
On the flip side, calming the nervous system activates the "rest and digest" state. This is where gentle, supportive strategies can play such a powerful role. Techniques that promote relaxation can help improve the body’s overall tone and function, easing the tension that so often contributes to silent reflux symptoms.
Chronic stress can keep the nervous system in a state of high alert, disrupting the delicate balance needed for healthy digestion. By focusing on stress reduction, we are directly supporting the body's ability to heal and regulate itself.
Supportive Neurological Care
Since the vagus nerve is the master controller for digestion, ensuring it can send and receive clear signals is absolutely crucial. Neurological interference, often stemming from physical stressors during the birth process or even developmental tumbles and falls, can disrupt this communication highway. The result can be poor coordination of the digestive system, including those sphincters that are supposed to prevent reflux.
Gentle, specific chiropractic care focused on the nervous system can help reduce this interference. By improving spinal alignment and motion—especially in the upper neck where the vagus nerve is housed—we can help restore proper nerve function. This enhances the brain's ability to regulate the digestive process effectively.
This approach doesn't "treat" the reflux itself; rather, it supports the body’s innate ability to control and coordinate its own systems. To better understand this connection, you can read our guide on stimulating the parasympathetic nervous system, which is the "rest and digest" system that optimal vagal function supports.
Bringing these supportive strategies together can create a powerful, holistic approach to managing silent reflux. Below is a table that summarizes some of these gentle but effective options for your family.
Holistic Management Strategies for Silent Reflux
| Strategy Area | For Infants & Children | For Adults |
|---|---|---|
| Dietary Support | Offer smaller, more frequent feedings. Keep a food diary to identify potential triggers in mom's diet (if breastfeeding) or the child's diet. Introduce solids carefully. | Avoid common triggers like spicy, acidic, and fatty foods. Eat smaller meals throughout the day instead of three large ones. Avoid late-night eating. |
| Lifestyle & Positioning | Keep baby upright for 20-30 minutes after feeding. Ensure proper latch during feeding to reduce air intake. Follow safe sleep guidelines—no wedges or positioners without medical advice. | Elevate the head of the bed by 6-8 inches. Wear loose-fitting clothing that doesn't constrict the abdomen. Maintain a healthy weight. |
| Stress & Neurological Health | Gentle massage, skin-to-skin contact, and a calm environment can soothe the nervous system. Gentle, neurologically-focused chiropractic adjustments can address physical stress. | Practice stress-reduction techniques like deep breathing, meditation, or light exercise. Ensure proper spinal alignment through chiropractic care to support vagus nerve function. |
Remember, the goal is not just to manage symptoms, but to support the body's overall function and promote long-term well-being.
When to Seek Immediate Medical Attention
While these supportive strategies are effective for managing many cases of silent reflux, certain "red flag" symptoms require immediate medical evaluation to rule out more serious conditions. It's vital to know when professional medical intervention is the right next step.
Always consult a specialist if you or your child experience any of the following:
- Breathing Difficulties: This includes any wheezing, apnea (pauses in breathing), or turning blue.
- Significant Weight Loss or Failure to Thrive: If an infant is not gaining weight as they should, or if an adult is losing weight without trying.
- Severe Pain: Intense, persistent chest or abdominal pain.
- Forceful or Projectile Vomiting: This can be a sign of a different condition, especially in infants.
- Blood in Spit-Up or Stool: Any sign of bleeding should be evaluated right away.
Navigating these red flags with confidence ensures you are taking the safest and most appropriate path for your family’s health.
Common Questions About Silent Reflux
Diving into the world of silent reflux can feel overwhelming, and it's completely normal for families to have a lot of questions. As you start connecting the dots between those subtle symptoms and this underlying condition, practical concerns naturally pop up. This section is here to give clear, straightforward answers to the questions we hear most often, helping you feel more confident moving forward.

Understanding what to expect on your family's path to relief is a huge part of the healing process. Let's tackle some of the most pressing queries we hear from families just like yours.
How Long Does It Take for Changes to Work
One of the very first questions people ask is, "How long until we see a difference?" The honest answer is that it really depends on the individual and the specific strategies you're using. But across the board, consistency is the single most important factor.
When you start making those key dietary and lifestyle adjustments, many people begin to notice a real reduction in their silent reflux symptoms within just a few weeks. The initial healing phase, where you’re really diligent about avoiding trigger foods, typically lasts about four to six weeks. This period gives the irritated tissues in the throat and larynx a chance to calm down and start repairing.
However, for symptoms to fully resolve, it can take several months of consistent management. It helps to remember that the goal isn't just a quick fix—it's about finding long-term balance and wellness.
Can Silent Reflux Cause Long-Term Damage
This is a very valid concern, especially if symptoms have been lingering for a while. If it's left unaddressed, the persistent exposure of those delicate throat and airway tissues to stomach contents can unfortunately lead to chronic problems down the road.
Some potential long-term complications can include:
- Chronic Laryngitis: This is a persistent inflammation of the voice box, which could lead to irreversible voice changes.
- Vocal Cord Damage: Over time, irritation can cause nodules or other lesions to form on the vocal cords.
- Increased Risk of Other Conditions: Ongoing irritation can contribute to recurring sinus or ear infections and may even worsen conditions like asthma.
The good news is that with proper management and supportive care, the risk of these complications is significantly reduced. Getting to the root cause is always the most effective way to protect long-term health.
How Is Silent Reflux Diagnosed Differently in Ages
The way silent reflux is diagnosed often changes with age, because the tools used and the symptoms themselves can look very different in an infant versus an adult.
For infants and young children, a diagnosis is frequently made based on a detailed health history and a close look at classic physical signs. A provider will look for patterns like back arching during feeds, persistent feeding difficulties, and chronic congestion. More formal testing is usually only brought in for severe cases or if any red flag symptoms appear.
In adults, the process can be more involved because the symptoms overlap with so many other conditions. An ear, nose, and throat (ENT) specialist might use a laryngoscopy—a procedure involving a tiny camera—to visually inspect the throat and voice box for the tell-tale signs of reflux-related inflammation. In some situations, a 24-hour pH monitoring test may be used to confirm the presence of acid in the upper airway.
At First Steps Chiropractic, we believe in empowering families with the knowledge and support they need to address health challenges from the ground up. If you are navigating the complexities of silent reflux and seeking a gentle, neurologically-focused approach to support your family's well-being, we are here to help. Schedule a consultation with us today.

