When parents first learn about the link between hypotonia and autism spectrum disorder, it often feels like a missing puzzle piece finally clicking into place. If you've ever held your baby and thought they felt a bit "floppy," or noticed your toddler seems to tire out faster than their peers, you're not just imagining things. This isn't a small side note; it's often one of the very first physical clues on a child's unique developmental path.
Understanding The Link Between Hypotonia and Autism

Hypotonia, the clinical term for low muscle tone, isn't a problem with the muscles themselves. It’s not about muscle weakness. A better way to think about it is with an analogy.
Imagine your child’s muscles are lightbulbs, and their nervous system is the wiring and the dimmer switch. For those lightbulbs to glow brightly and consistently, they need a strong, steady signal from the switch.
If the signal is weak or inconsistent—like the dimmer is turned way down—the lights will be dim or might even flicker. In a child with hypotonia, the nervous system struggles to send those strong, constant signals that tell the muscles how much tension to hold at rest. The result is muscles that feel soft or "floppy" to the touch, all stemming from that inefficient brain-to-body communication.
Why The Connection Matters
Recognizing this connection is a game-changer because motor challenges are often noticeable long before the social and communication differences associated with autism become clear.
This early physical sign is incredibly valuable. In fact, research shows just how common it is. Some studies suggest that around 50% of children on the autism spectrum have hypotonia. One large analysis of over 5,000 children found that the presence of hypotonia led to an ASD diagnosis 1.5 years earlier, on average. You can dig deeper into how hypotonia impacts diagnosis timelines at Strides ABA.
For parents, noticing signs of low muscle tone isn't a reason to panic. It's an opportunity to be proactive. Your observations are powerful and can open the door to a full developmental evaluation, unlocking essential support services for your child much sooner.
What to Look For
So, what does hypotonia actually look like day-to-day? Knowing the signs at different stages can help you connect the dots and advocate for your child more effectively.
For parents trying to piece together what they're seeing, this quick reference table breaks down some of the common indicators of hypotonia in infants and toddlers.
Early Hypotonia Signs in Infants and Toddlers
| Developmental Stage | Common Hypotonia Indicators |
|---|---|
| Infants (0-12 months) | • Feels limp or like a "rag doll" when held • Difficulty lifting or controlling their head • Struggles with sucking and swallowing during feeding • Delayed rolling over or sitting up |
| Toddlers (1-3 years) | • Sits in a "W" position for extra stability • Seems clumsy or falls more often than peers • Delayed crawling, cruising, or walking milestones • Prefers sedentary play; tires easily during physical activity |
| Young Children (3+ years) | • Slumps or slouches in chairs; struggles to sit upright • Poor endurance; may ask to be carried often • Difficulty with fine motor tasks like buttoning, zipping, or holding a pencil • May walk with a wide-based or flat-footed gait |
Remember, every child develops at their own pace, but seeing these signs as potential indicators of an underlying hypotonia autism spectrum disorder connection is the first empowering step toward building the right support system for your child's journey.
Why Low Muscle Tone Is An Early Clue for Autism
When you’re a new parent, you’re watching for all those big, exciting milestones—that first real smile, the first coos and babbles, and of course, crawling and walking. These aren't just sweet photo ops; they're the most visible signs that a child's brain and nervous system are growing and connecting at an incredible rate. A child’s motor skills, in particular, give us one of the earliest and clearest windows into that complex brain-body connection.
Think of it like building a house. Long before you're picking out paint colors, you see the foundation being poured and the electrical wiring being run through the frame. Early motor skills are a lot like that foundational framework. If we see struggles here, it can sometimes be a sign that the underlying "wiring"—the nervous system—is developing a bit differently.
This is exactly why the link between hypotonia and autism spectrum disorder is so critical for parents and providers to understand. Low muscle tone isn't just about having "floppy" arms and legs. It's a real, physical clue that can point toward broader neurodevelopmental patterns and give us insight into how a child’s brain is sending and receiving messages from the very start.
The Brain-Body Connection at Play
When a baby feels a little too limp in your arms or a toddler struggles with tasks that require strength and coordination, it’s often a direct reflection of inefficient neurological signaling. The brain is sending out commands, but they might be arriving at the muscles with less intensity, kind of like a radio signal that's full of static. This same neurological signature—one built on differences in processing and communication—is often at the core of autism spectrum disorder.
Now, having hypotonia doesn't automatically mean a child has or will have autism, but it’s a powerful reason to look closer. It often serves as the catalyst for the kind of in-depth neurodevelopmental evaluations that might otherwise not happen until social or behavioral signs become more obvious down the road. Getting a head start on that investigation is absolutely crucial for getting support in place early.
Hypotonia in infancy can be more than just a motor delay; it is often one of the first visible indicators of the unique neurodevelopmental path associated with autism, prompting a closer look at a child's entire developmental trajectory.
Research Confirms the Early Warning Link
A growing mountain of research is confirming what developmental specialists have seen in practice for years: early motor challenges are frequently a precursor to a later autism diagnosis. This isn't a reason to panic—it's an opportunity. By recognizing hypotonia, parents and doctors can shift from a passive "wait-and-see" approach to a much more proactive "investigate-and-support" mindset.
This proactive stance can make all the difference in how early a child gets diagnosed and starts accessing therapies that can help. The presence of hypotonia acts as a powerful 'red flag' for autism spectrum disorder, often leading to diagnoses much sooner. In one pivotal study of 1,182 children with ASD, hypotonia significantly lowered the age of diagnosis. For boys, it led to a diagnosis up to 1.5 years sooner than their peers without low tone. You can dive into the details in the full research study on early diagnosis.
Empowering Parents Through Observation
Understanding this connection is incredibly empowering. It turns your parental worries into valuable, actionable information. When you notice your child is constantly slumping, seems to be missing motor milestones, or just feels unusually "heavy" or limp when you pick them up, you’re not just seeing a physical quirk. You are gathering key data about their neurological development.
This knowledge equips you to have much more specific and productive conversations with your pediatrician. Instead of just saying, "Something feels off," you can point to concrete examples of low muscle tone. This clarity helps ensure your concerns are taken seriously, opening the door to the right assessments and therapies that will help your child build strength, coordination, and confidence. No time is lost in getting them the support they need to truly thrive.
The Neurological Roots of Low Muscle Tone in ASD
To really understand the link between hypotonia and autism spectrum disorder, we have to look past the muscles and go straight to the source: the body’s master control system. The nervous system. It’s a common misconception that low tone is a muscle problem, but the muscles themselves are usually just fine. The real issue is rooted in the messages—or lack thereof—that they’re receiving from the brain.
Think of the nervous system as a complex communication network, with the brain acting as the central command tower. This tower is constantly firing off signals through intricate wiring to every corner of the body. These signals tell our muscles exactly how much tension to hold at all times, even when we’re just sitting still.
In a child with hypotonia, this communication network has a few glitches. The signals traveling from the brain to the muscles can be weak or inconsistent, almost like a spotty Wi-Fi connection that keeps dropping. As a result, the muscles aren't kept in that constant state of readiness, which leads to that classic "floppy" or overly relaxed feeling.
Unpacking the Brain-Based Signaling Challenge
So, this isn’t about muscle weakness—it’s a challenge of neurological signaling. Specific areas of the brain, especially the cerebellum, are mission control for coordinating movement, balance, and motor planning. We know from research that in many kids with ASD, these key brain regions function a bit differently, which directly affects how motor commands are sent out and carried through.
This difference in brain function is a huge piece of the puzzle, explaining why hypotonia shows up so often in kids on the spectrum. It's a direct, physical expression of their unique neurodevelopment. When parents grasp this, it helps shift the focus; low muscle tone isn't some separate, isolated problem but an integral part of their child's neurological wiring.
The infographic below shows how spotting hypotonia can kickstart a journey that goes from neurological evaluation to a much earlier autism diagnosis.
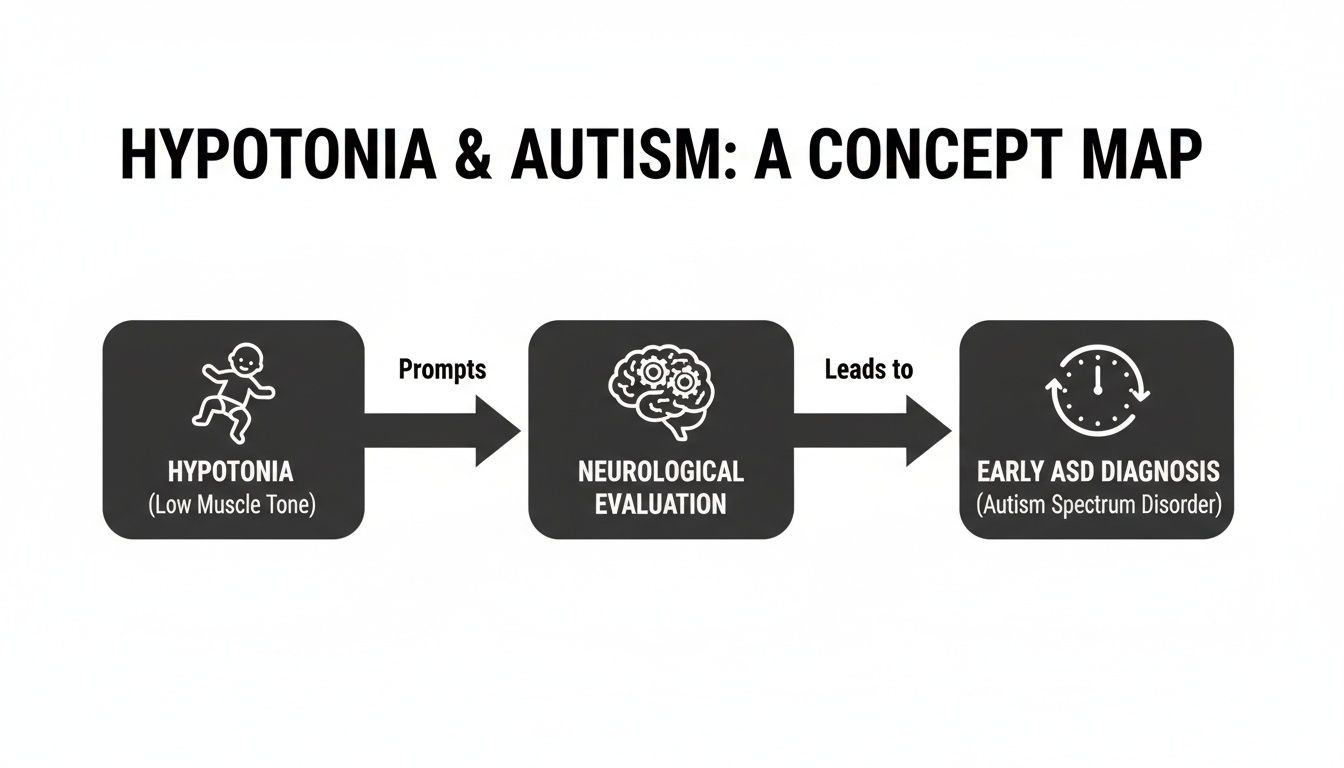
This visual flow makes it clear how a physical sign like low muscle tone can be a critical gateway to a full neurodevelopmental workup and, most importantly, timely support.
The Impact on Motor Milestones and Beyond
This inefficient brain-muscle signaling has a major ripple effect. It often contributes to delays in hitting motor milestones and can make it harder for a child to explore and interact with their world. In fact, startling new data reveals that approximately 50% of children with ASD experience hypotonia. This neurological-motor connection is so significant that it can even predict future outcomes; for example, fine motor scores at six months can forecast language abilities at age three. You can dive deeper into how motor skills predict later abilities at Frontiers.
Because the root of the problem is neurological, it stands to reason that the most effective support strategies are the ones that address the nervous system directly. This is exactly where specialized pediatric care makes a difference by offering a foundational approach that improves this core communication network.
By focusing on the nervous system, we can help improve the clarity and strength of the brain's signals to the body. This approach doesn't just manage symptoms; it addresses the root cause of the motor challenges associated with hypotonia.
A Neuro-Tonal Approach to Care
At First Steps Chiropractic, our entire approach is built on this principle. We use gentle, specific, and neurologically-focused techniques designed to clear up the communication pathways between the brain and body. The goal is simple: reduce interference within the nervous system so those crucial signals can get through loud and clear.
By improving this "communication highway," we can help strengthen the brain-muscle connection. For many kids, this translates to better muscle tone, improved coordination, and more stable posture. You can learn more about how we support the connection between autism and the nervous system in our detailed guide.
This neuro-tonal approach works hand-in-hand with traditional therapies like PT and OT. By improving the body's foundational control system, we help create a more stable platform for a child to build strength, master new skills, and truly thrive.
How Low Muscle Tone Affects Daily Life

Knowing the clinical term "hypotonia" is one thing, but seeing how it actually shows up in your child's world is what truly matters. Low muscle tone isn't just about being a little less coordinated; it creates a ripple effect that touches nearly every part of a child's development.
Imagine trying to build a LEGO tower while wearing a pair of floppy, oversized gloves. That’s a small glimpse into the enormous extra effort a child with hypotonia has to put into tasks that seem simple to others.
This constant physical battle shapes how they explore, learn, and connect. When a child's muscles lack that baseline, ready-to-go tension, even something as basic as sitting up straight at the dinner table requires a huge amount of concentration and energy. The challenges go way beyond just hitting milestones a little later—they influence how a child plays, participates in school, and builds their confidence.
Gross Motor And Postural Challenges
Gross motor skills are all about the big muscles we use for walking, running, jumping, and balancing. For a child with hypotonia autism spectrum disorder, these movements can look clumsy or uncoordinated. This isn't because they're being careless; it's because their body has to work overtime just to stay stable.
You might notice this in a few key ways:
- A "W-Sitting" Habit: Many toddlers with low tone sit with their legs splayed out in a "W" shape. This gives them a wider, more stable base of support so they don't have to work their core muscles as hard.
- Frequent Tripping And Falling: Poor core stability and coordination can lead to lots of stumbles. For these kids, the playground can feel more overwhelming than fun.
- Low Endurance: Does your child ask to be carried long after their friends are still running around? That’s not laziness. Their muscles get tired much faster, turning a short walk into an exhausting marathon.
- Slumped Posture: Holding an upright posture in a chair or on the floor is a constant fight against gravity. Slouching is simply their body's way of conserving precious energy.
These visible struggles are directly connected to those neurological signals we talked about earlier. To learn more about how to build these foundational skills, check out our guide on supporting healthy gross motor development.
To better understand how these challenges translate into real-world situations, the table below breaks down the impact of low muscle tone across different activities.
Hypotonia's Impact Across Different Activities
| Activity Area | Examples of Challenges | Long-Term Implications |
|---|---|---|
| Playground Fun | Difficulty climbing ladders, swinging, or keeping up with peers in a game of tag. May avoid physically demanding activities. | Social isolation, reduced physical fitness, and missed opportunities for peer interaction and skill-building. |
| Classroom Participation | Slouching at a desk, struggling to sit still during circle time, and having trouble carrying a lunch tray or backpack. | Difficulty focusing, being perceived as inattentive, and challenges with school routines that require physical stamina. |
| Self-Care Tasks | Trouble with dressing (buttons, zippers), brushing teeth, and using a knife and fork. Mealtimes can be messy and slow. | Delays in independence, frustration with daily routines, and reliance on caregivers for tasks peers can do themselves. |
| Creative Play | Avoiding activities like building with small blocks, coloring within the lines, or doing crafts that require precise hand movements. | Reduced opportunities to develop creativity, problem-solving skills, and the fine motor control needed for handwriting. |
Seeing these patterns helps connect the dots between specific behaviors and the underlying issue of hypotonia, making it easier to target the right kind of support.
Fine Motor Skill Difficulties
Hypotonia also has a big impact on the small, precise muscles in the hands and fingers, which can make fine motor tasks a major source of frustration. When a child has to pour all their energy into just holding a crayon, the simple joy of coloring can vanish.
It's essential to recognize that for a child with low muscle tone, tasks like writing or buttoning a shirt can be as physically demanding as an intense workout is for an adult. This perspective transforms our understanding from seeing a "struggle" to seeing incredible effort.
This difficulty often looks like this:
- A Weak Or Awkward Pencil Grip: This can make handwriting messy, oversized, or barely readable.
- Trouble With Fasteners: Buttons, zippers, and snaps remain a big challenge long after their friends have mastered them.
- Difficulty With Utensils: Holding a fork or spoon correctly can be tricky, leading to messy and frustrating mealtimes.
- Avoiding Certain Toys: You might notice they shy away from activities that require precise hand movements, like stringing beads or playing with small LEGOs.
When you start connecting these different daily challenges, you can see how they all stem from the same root cause: low muscle tone. Gaining this clarity is the first real step toward finding the right support to help your child build strength and navigate their world with more confidence and ease.
Building a Strong Support System for Your Child
Spotting the signs of low muscle tone is the first, crucial step. The next is to bring together a dedicated team of professionals who can provide targeted, evidence-based support for your child. The goal isn’t to "fix" the hypotonia; it's about empowering your child with the strength, coordination, and confidence they need to thrive in their world.
The best results almost always come from a collaborative strategy. When you bring together specialists who understand the different ways hypotonia and autism spectrum disorder can impact a child's development, you create a powerful synergy. This team approach provides well-rounded care that turns daily struggles into major wins.
The Core Therapeutic Team
A few key therapies are the bedrock of support for any child with low muscle tone. Each one plays a unique but deeply connected role in building essential life skills. Think of them as different coaches, each one honing a specific aspect of your child’s abilities.
- Physical Therapy (PT): This is where gross motor skills get a workout. A physical therapist is like a personal trainer for your child’s bigger muscle groups, focusing on things like core strength, balance, and coordination. The best PT sessions feel just like playtime, using obstacle courses, therapy balls, and balance beams to make getting stronger fun.
- Occupational Therapy (OT): While PT is busy with the big movements, OT focuses on the fine motor skills and sensory processing that are so important for everyday life. An occupational therapist helps kids master the "jobs" of childhood—like buttoning a shirt, holding a crayon correctly, or using a fork and knife. They build the functional skills that lead directly to more independence.
- Speech-Language Pathology (SLP): Hypotonia doesn't just affect the limbs; it can also impact the small, intricate muscles of the face, jaw, and tongue. An SLP is the expert here, working to improve oral-motor control, strengthen these muscles for clearer speech, and address feeding challenges like chewing and swallowing.
A Complementary Neurological Approach
These traditional therapies are absolutely essential for building functional strength and skills. But since hypotonia is fundamentally rooted in how the nervous system communicates with the muscles, it just makes sense to support that master control system directly. This is where a neurologically-focused pediatric chiropractic approach can be an invaluable addition to your child's team.
It’s really important to be clear: this type of chiropractic care does not treat autism or hypotonia. Its primary goal is entirely different—it's focused on optimizing the function of the central nervous system. By using gentle, specific adjustments, the aim is to reduce any interference in the communication pathways between the brain and the body.
Think of the nervous system as a highway. If there are traffic jams or roadblocks, messages can't get through quickly or clearly. By clearing those pathways, we help ensure the brain's signals to the muscles are as strong and efficient as possible.
This approach works to create a more stable and organized neurological foundation. When a child's internal signaling is working better, they are often in a much better position to build strength, learn new motor patterns, and get more out of every single PT and OT session. It supports the very systems that other therapies are working so hard to train.
When you combine the skill-building work of PT and OT with care that supports the underlying nervous system, you create a truly powerful and comprehensive plan. This integrated approach addresses both the symptoms and the root cause of the motor challenges, giving your child a robust support system to help them reach their full potential.
How Neurologically-Focused Chiropractic Care Helps

While traditional therapies are absolutely essential, it’s worth remembering that the challenges of hypotonia autism spectrum disorder are rooted in the nervous system. So, it just makes sense to support that master control system directly. This is where neurologically-focused pediatric chiropractic care comes in, offering a foundational approach that complements therapies like PT and OT beautifully.
Let's be clear: this specialized form of chiropractic care doesn’t treat or cure autism or hypotonia. Its entire focus is on optimizing the function and regulation of the nervous system—the body's central command center for everything from motor control to sensory processing.
Think of the nervous system as a highway. Stressors, especially from birth trauma or spinal misalignments, can create "traffic jams" (we call these subluxations) that mess with the flow of information. For a child with low muscle tone, these interruptions can mean the brain's signals telling the muscles to stay "on" and ready for action are weak or inconsistent.
Restoring The Brain-Body Connection
Neurologically-focused pediatric chiropractic is a world away from the adjustments you might imagine for an adult. We use incredibly gentle and precise adjustments designed specifically for a child’s delicate, developing nervous system. These adjustments help reduce interference, clearing those communication pathways.
It’s like turning a bumpy, congested road into a smooth, multi-lane freeway. When the brain-body communication improves, the brain can coordinate all of the body's functions more effectively, including maintaining proper muscle tone. This can kickstart a positive ripple effect, supporting the very systems that other therapies are working so hard to build.
By addressing underlying neurological stress, pediatric chiropractic care helps set the stage for other therapies to be more effective. When the body's internal signaling is clearer, a child is better equipped to build strength, learn new motor patterns, and improve coordination.
The Care Process From Start To Finish
Knowing what to expect can make this supportive approach feel much more approachable. The journey is carefully mapped out to give us a crystal-clear picture of your child's unique neurological state.
Here’s what the process usually involves:
- In-Depth Consultation: We start by listening. This is our chance to learn all about your child's health history, your specific concerns, and what your family is hoping to achieve.
- Advanced Insight Scans: We use state-of-the-art, non-invasive technology to map out areas of stress and dysregulation in the nervous system. These scans give us objective data that shows us exactly where interference is happening.
- Personalized Care Plan: Based on our conversation and the scan results, we create a specific, customized care plan for your child. No two plans are ever the same because no two nervous systems are.
This detailed process ensures that care is tailored to your child’s exact needs. By improving the function of the body’s master control system, we aim to enhance motor control, improve sensory processing, and support overall development. To explore this topic further, you can learn more about how autism chiropractic care supports the nervous system. This foundational strategy helps create a more stable neurological platform, empowering your child to get the most out of every therapy and life experience.
Common Questions About Hypotonia and Autism
Navigating the world of hypotonia and autism spectrum disorder naturally brings up a lot of questions. Getting clear, straightforward answers is a huge part of feeling confident as you support your child, so let's tackle some of the most common concerns parents bring to us.
Understanding these key points can help you advocate for your child more effectively and build the right support team from day one.
Can a Child Have Hypotonia Without Autism?
Yes, absolutely. Hypotonia can show up all on its own—sometimes called benign congenital hypotonia—or it can be a sign of other underlying conditions. It's not exclusive to autism.
However, its high prevalence in children on the spectrum, affecting around 50% of them, makes it a critical flag. If you see signs of low muscle tone, it's a strong signal that a comprehensive developmental evaluation is a good next step. This helps you see the whole picture, ensuring your child gets the right support for their specific needs, whether that includes an ASD diagnosis or not.
Will My Child Outgrow Low Muscle Tone?
This is a question that comes straight from the heart, and it's an important one. The honest answer is that the underlying low muscle tone is typically a lifelong characteristic. It's fundamentally tied to how the nervous system is wired, so it isn't something a child simply outgrows like a pair of shoes.
But that's not the end of the story. The goal of therapies like PT, OT, and neurologically-focused chiropractic care is not to 'cure' hypotonia. Instead, we focus on building incredible functional strength, coordination, and stability so your child can thrive.
Through consistent and targeted support, kids learn to compensate beautifully. They build strength in a way that works for their body, which can dramatically reduce the impact hypotonia has on their daily life and activities.
What Is the First Step If I Suspect Hypotonia?
Trust your gut. As a parent, you have an instinct that is incredibly powerful. Your first and most important step is to bring your concerns to your pediatrician.
When you go, try to be specific. Instead of just saying something feels "off," give them concrete examples. Mention things like, "He feels floppy when I pick him up," or "She struggles to hold her head up during tummy time." The more detail, the better.
From there, your doctor can do an initial check and refer you to a team of specialists for a deeper look. This team often includes:
- A developmental pediatrician or a pediatric neurologist
- A physical therapist (PT) to assess gross motor skills like sitting and crawling
- An occupational therapist (OT) to look at fine motor skills and daily living tasks
How Can I Help My Child at Home?
Your role at home is huge! Creating a playful and encouraging environment is one of the best ways to reinforce all the hard work your child does in therapy.
Your therapists will give you a specific home exercise program tailored to your child. The real magic happens when you weave these activities into your daily routine so it doesn't feel like work. Think fun tummy time for babies, building obstacle courses in the living room for toddlers, or getting creative with Play-Doh and drawing for fine motor practice. The key is to keep it light and fun, which builds both strength and confidence.
At First Steps Chiropractic, we specialize in neurologically-focused care that supports the brain-body connection, helping your child get the most out of their therapies. To learn how we can be a part of your child's support team, schedule a consultation with us today.

