You've probably heard a birth story or two where someone mentions the baby was born "sunny side up." It’s a sweet-sounding term for what's known medically as the occiput posterior (OP) position. But as charming as it sounds, this specific fetal position can bring some real challenges to labor and delivery.
A baby born face up often means a longer, more difficult labor, frequently marked by intense back pain. It also increases the chances of needing medical interventions, from an epidural to get through the pain to assistance from forceps, a vacuum, or even a Cesarean section.
What It Means When a Baby Is Born Face Up
To really get what's happening, it helps to picture your pelvis as a curved tunnel. For the smoothest, most efficient journey, a baby needs to tuck their chin and present the smallest part of their head, with their face pointing down toward your spine. This ideal setup is called the occiput anterior (OA) position.
When a baby is in the face-up, or OP position, they're still head-down, but their face is looking up at your abdomen. This simple flip means a wider part of their head has to navigate the tight corners of your pelvic bones. As you can imagine, this can make for a longer and more strenuous trip for both of you.
Understanding Fetal Positions
Not all head-down positions are created equal. That subtle difference in how a baby's head is oriented can impact everything from how long labor lasts to whether you need help with the delivery.
This concept map breaks down the difference between the optimal (OA) and face-up (OP) positions perfectly.
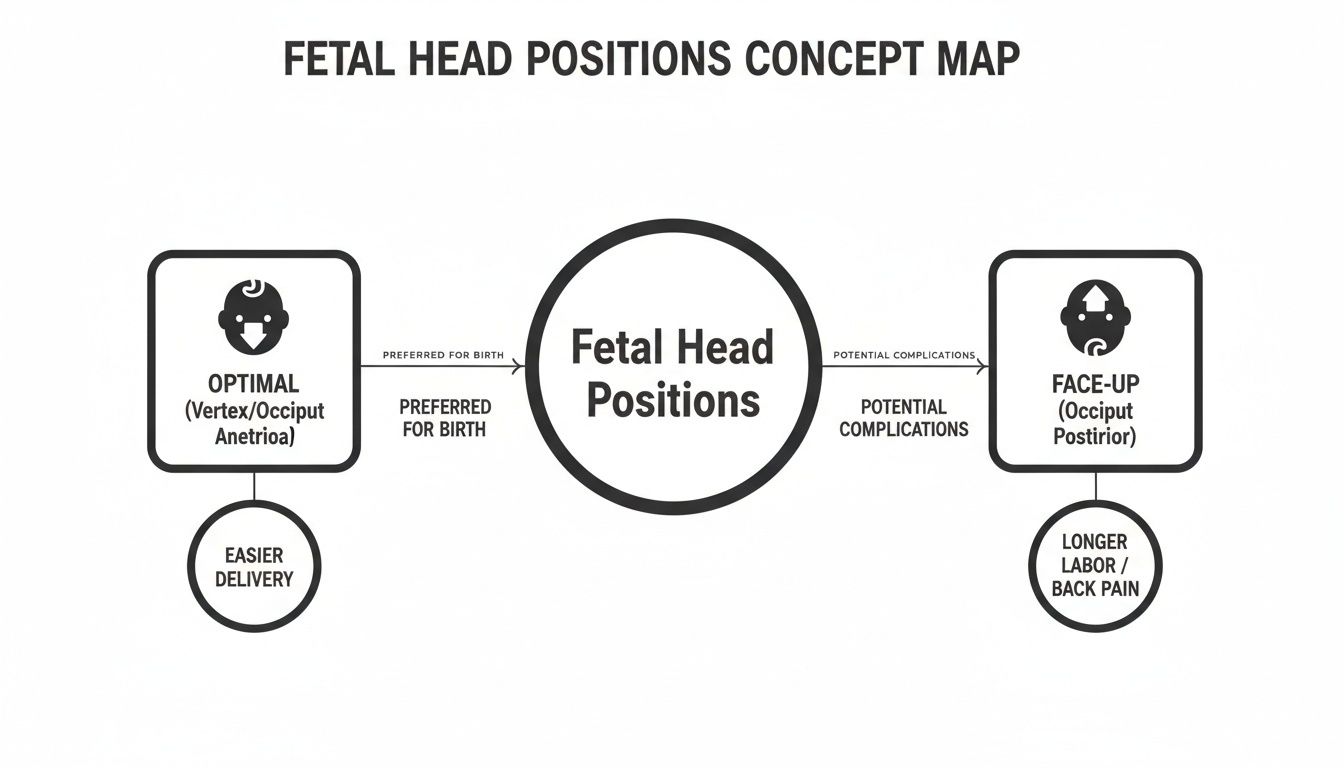
You can see right away how the baby's head alignment changes the whole dynamic, making one path much smoother than the other.
How Common Is the Face-Up Position?
Here's the good news: while many babies start labor in a face-up position, most of them will actually rotate on their own during contractions, shifting into the better OA position before it's time to push.
It's the baby who stays face-up all the way through delivery that can lead to complications. This is less common than you might think, but it happens often enough that your birth team is ready for it. For perspective, other non-optimal positions like breech (feet-first) happen in about 3-5% of full-term pregnancies. You can dig deeper into the global incidence of fetal presentation in recent studies.
The key takeaway is that while many babies may be face up at some point, only a small fraction stay that way for the actual delivery. Your body and your baby are designed to work together, and often, this issue corrects itself.
Fetal Head Positions At A Glance
To make it even clearer, let's compare the two main head-down positions side-by-side. This table really helps show why one is "optimal" and what makes the other more of a challenge.
| Feature | Optimal Position (Occiput Anterior) | Face-Up Position (Occiput Posterior) |
|---|---|---|
| Baby's Facing Direction | Toward the mother's spine | Toward the mother's abdomen |
| Head Diameter | Smallest part of the head leads | Larger part of the head leads |
| Labor Progression | Typically smoother and faster | Often results in slower progress and longer labor |
| Common Sensation | Contraction pain felt in the abdomen | Intense, persistent "back labor" is common |
| Need for Intervention | Lower likelihood of intervention | Higher likelihood of needing assistance (e.g., vacuum, forceps) |
Grasping this fundamental difference is the first step in feeling prepared for whatever your labor brings. It empowers you to ask the right questions and work as a team with your providers.
Understanding the Complications for Mothers
When your baby is positioned face up, the journey through labor can feel a lot more like an uphill battle. This position, known as occiput posterior (OP), doesn't just shift your baby's angle; it can fundamentally change the entire labor experience. These potential complications aren't just statistics—they're real, physical hurdles that can make the process more intense and exhausting.
Knowing what these challenges are isn't meant to scare you. It’s all about building awareness so you can feel prepared, ask the right questions, and be your own best advocate during one of the most important days of your life.

The Challenge of Back Labor
One of the most talked-about and toughest parts of a face-up labor is the infamous "back labor." This isn't the typical tightening and releasing of contractions felt across the abdomen. Instead, back labor is often a deep, severe, and relentless ache in the lower back. This intense pressure happens because the hardest part of your baby’s skull is pressing directly against your sacrum—the triangular bone at the very base of your spine.
This constant pressure often doesn't let up between contractions, giving you little to no break. It can be incredibly draining, both physically and emotionally, making it much harder to cope as labor progresses. Learning how to manage this pain is key, and you can find some excellent strategies in our guide to prenatal exercises for back pain, many of which can be adapted for labor.
Why Labor Can Last Longer
A face-up baby often means a longer, less efficient labor. Think of it this way: to move down the birth canal, a baby's head needs to tuck its chin and rotate to fit through the pelvis. When face up, the baby's head is in a less-than-ideal position to make these critical moves.
This can cause a few specific delays:
- Slower Dilation: The pressure from a baby's head on the cervix is a primary trigger for dilation. In an OP position, that pressure is often less direct and effective, which can slow everything down.
- Prolonged Pushing Stage: Even after you've finally reached full dilation, the pushing stage can drag on. Some studies show the second stage of labor can be, on average, an hour longer for mothers whose babies remain in the OP position.
- Maternal Exhaustion: A longer labor, especially one paired with intense back pain, is profoundly tiring. This fatigue can make the final push even more difficult, sometimes weakening the effectiveness of a mother's efforts.
A longer labor is not a reflection of your strength or effort. It's a simple mechanical issue—the baby just has a tougher path to travel, and it takes more time and work from both of you to get there.
Higher Rates of Medical Intervention
Because of these added challenges, a face-up birth often comes with a higher chance of needing some medical help. Your care team’s number one goal is a safe delivery for you and your baby, and they have tools to assist when labor stalls or becomes too much.
Instrumental Delivery
When the baby needs a little extra help navigating the final stretch, especially after a long pushing stage, your doctor might suggest an assisted delivery. This means using special tools to gently guide the baby out.
- Forceps: These look like large, curved tongs that are carefully placed around the baby’s head to help with rotation and descent.
- Vacuum Extractor: This uses a soft cup that attaches to the baby’s head with suction, allowing the provider to help pull during contractions.
While these tools are very effective at ensuring a safe birth, they are used more often when a baby is face up simply because of the difficulty of that final descent.
Increased Risk of Perineal Tears and C-Section
The wider diameter of the baby's head pressing against the perineum (the tissue between the vagina and anus) can increase the chances of tearing during delivery. More severe tears, known as third- or fourth-degree lacerations, are unfortunately more common with OP births.
Finally, if labor just won't progress despite everyone's best efforts, or if there are any signs of distress, an unplanned Cesarean section might become the safest path forward. The rate of C-sections is significantly higher for persistent OP positions—some studies report it reaching as high as 50%, a stark contrast to the much lower rate for babies in the optimal head-down position. This change in the birth plan is always made with one thing in mind: the health and safety of both mom and baby.
What This Means for Your Baby
Just as a face-up birth can be more demanding for mom, it's a tougher journey for the baby, too. While the vast majority of babies born in this position are perfectly healthy, the longer, more strenuous labor can sometimes lead to a few temporary issues. Your medical team is completely prepared for this, but knowing what to look for can help you feel more prepared in those first moments after birth.
The focus immediately shifts to your newborn and making sure their transition to the outside world is a smooth one. This initial check-up happens quickly and efficiently, with a dedicated team ready to give your baby any support they might need. The good news is that these potential complications are almost always short-lived, resolving within a few hours or days with expert care.

Apgar Scores Explained
Right after birth, at one and five minutes, your baby will be given an Apgar score. Think of it not as a test they pass or fail, but as a quick health checkup. It assesses five key signs: heart rate, breathing, muscle tone, reflexes, and skin color. A score between 7 and 10 is considered normal.
Babies who’ve had a longer, more stressful labor—like many who arrive face-up—might have a slightly lower score at first. This is often just due to the extra exertion and means they may need a little boost, like gentle stimulation or some oxygen, to get going. By the five-minute check, most scores improve significantly as the baby adjusts.
Understanding Minor Birth Trauma
The journey through the birth canal is a tight squeeze, and a baby born face-up can show a few physical signs of their trip. Because their head was pressing against your pelvic bones, you might notice some temporary cosmetic issues that look more alarming than they actually are.
Common signs you might see include:
- Facial Bruising: Since the baby's face, not the back of their head, led the way, some minor bruising can occur.
- Swelling or "Molding": Your baby's head might look a bit cone-shaped or swollen. This is a normal process that helps them fit through the pelvis and typically goes back to normal within a day or two.
- Caput Succedaneum: This is simply swelling on the scalp, common after a long labor or a vacuum-assisted delivery. It's just fluid under the skin and disappears on its own.
Your pediatric team will be monitoring these superficial issues closely. It's also worth noting that the physical stress of birth can sometimes lead to subtle misalignments in a newborn's spine. This is an area where gentle pediatric chiropractic care can offer support for their overall comfort and nervous system function. You can learn more about chiropractic care for babies and how it can help after a tough delivery.
While a difficult birth position can increase certain risks, it's important to frame this in a broader context. For instance, even with more complex presentations like breech, medical advancements ensure high safety standards. A 2022 meta-analysis found the risk of perinatal mortality for a planned vaginal breech delivery was about 0.6%, highlighting how care teams manage higher-risk situations. For more details on this topic, you can read the full research about delivery methods.
Brief Stays in the NICU
In some cases, a baby who has had a particularly challenging birth might need a short period of observation in the Neonatal Intensive Care Unit (NICU). This is usually just a precautionary measure, not a sign of a serious, long-term problem.
A stay in the NICU might be recommended for a few reasons:
- Breathing Support: If the baby is having a little trouble clearing fluid from their lungs or their breathing is still a bit labored.
- Monitoring: To keep a close eye on heart rate, oxygen levels, or blood sugar after a long and stressful labor.
- Low Apgar Scores: If the initial Apgar score was very low and the baby needed a bit more help to stabilize.
Usually, this is a very brief stay—just long enough for the medical team to be certain your baby is stable and thriving. This extra level of care is there to provide peace of mind and ensure your little one gets the best possible start.
How Doctors and Midwives Manage a Face Up Labor
When your care team realizes your baby is in a face-up, or occiput posterior (OP), position, their focus immediately shifts to a proactive and deeply supportive mode. The main goal is to gently encourage your baby to rotate into a better position for birth, all while keeping a close eye on the health and safety of both of you.
This isn't about jumping to one single solution. It's more like a responsive dance between you, your baby, and your birth team, starting with the simplest, least invasive strategies and only moving on to others if they become necessary. They’ll be constantly observing and suggesting adjustments to help things move along.
Starting with Non-Invasive Techniques
Before anyone even thinks about medical interventions, the first step is always to use gravity and movement to your advantage. Your doctor or midwife essentially becomes your personal labor choreographer, suggesting different positions to help create more space in your pelvis.
Sometimes, that little bit of extra room is all your baby needs to make that crucial turn. These aren't just random movements; they are proven techniques designed to open your pelvis asymmetrically, giving your baby the best possible chance to find a better path.
You might be guided through positions like:
- Hands and Knees: A classic for a reason! This position takes all the pressure off your back and lets gravity do the work, helping the heaviest part of your baby (their back) swing forward toward your belly.
- Side-Lying with a Peanut Ball: Lying on your side with a peanut-shaped ball wedged between your knees is a game-changer for opening up the pelvic outlet. Simply switching from one side to the other can be enough to encourage rotation.
- Lunges and Asymmetrical Poses: Things like leaning into a lunge or putting one foot up on a stool create an uneven pelvic alignment. This can be just the trick to help a "stuck" baby find a new way to move down.
Your body is designed for this. Often, all it takes is a simple shift in your position to give your baby the space and encouragement they need to rotate. Your care team is there to guide you through these movements safely.
Managing Pain and Providing Support
One of the biggest challenges with a face-up baby is the intense back labor that often comes with it. Getting this pain under control is not just about your comfort—it’s about your stamina. When you aren't overwhelmed by pain, you have so much more energy to move, change positions, and work with your body.
Your team will offer a whole range of pain management options that fit your needs and birth plan. This could be anything from hands-on counter-pressure massage on your lower back to sterile water injections, which can offer amazing (though temporary) relief from that deep ache.
For many, an epidural becomes a powerful tool. It can provide the significant relief needed for your body to relax, which can, in turn, help labor progress more effectively, especially when you're feeling exhausted.
When Medical Intervention Is Needed
If positional changes and giving it time don't do the trick, your provider might suggest more direct interventions. These decisions are never made lightly. They are always discussed with you, weighing the benefits against the risks so you can make an informed choice.
The first step is often a manual rotation. This is where a skilled doctor or midwife reaches into the birth canal during an exam and uses their hand to gently guide the baby’s head into a better position. It's usually done between contractions and can be incredibly effective, sometimes completely turning around a stalled labor.
If your baby still isn't rotating and the pushing stage becomes difficult, an instrumental delivery might be the next step. This means using forceps or a vacuum extractor to help guide the baby out, especially when a mother is exhausted after a long time pushing.
While the idea of instruments can sound scary, they are used with great care and precision to avoid the need for an emergency C-section. A Cesarean delivery is always the final option, reserved for situations where labor isn't progressing or if there are any signs of distress, ensuring the safest possible outcome for you and your baby.
To make sense of these options, here is a quick overview of how your team might approach an OP labor.
Management Options For Occiput Posterior Labor
| Strategy Type | Examples | Goal |
|---|---|---|
| Positional Changes | Hands and knees, side-lying with a peanut ball, lunges | Use gravity and movement to open the pelvis and encourage the baby to rotate naturally. |
| Pain Management | Counter-pressure, sterile water injections, epidural | Reduce intense back labor pain to conserve energy and help the body relax. |
| Manual Rotation | Provider uses a hand to gently turn the baby's head | Directly assist the baby into a more optimal (face-down) position. |
| Instrumental Delivery | Forceps, vacuum extractor | Assist the baby's descent during the pushing stage if the mother is exhausted or progress stalls. |
| Cesarean Delivery | Surgical birth | Ensure a safe delivery if labor is not progressing or if there are signs of fetal or maternal distress. |
Ultimately, your birth team has many tools and techniques to help navigate a face-up labor, always with the shared goal of a safe and healthy delivery for you and your baby.
Encouraging Optimal Fetal Positioning Before Labor

While your baby will be the one to make the final call on their birth position, you have a lot more influence than you might think. You can actively create an environment that encourages them to settle into that ideal anterior (face-down) position.
The goal isn't to force your baby into a specific spot. It’s about releasing tension in the muscles and ligaments supporting your uterus and pelvis. Think of it as making your baby’s first home as balanced and inviting as possible. When those structures are aligned and relaxed, your baby has the freedom to find the path of least resistance—which is almost always the optimal position for birth.
The Power of Posture and Movement
Our modern lives often involve long hours sitting in cars or at desks, leading to tight hip flexors and a tucked pelvis. This posture can actually make it more difficult for a baby to engage properly for labor. The good news is that by consciously adjusting how you move and rest, you can counteract these effects.
Simple, consistent postural awareness is your most powerful tool. The main idea is to keep your hips higher than your knees whenever you're seated. This simple shift helps tilt your pelvis forward, creating more space in the back of the pelvis and inviting your baby’s back (their heaviest part) to swing forward.
Here are a few easy adjustments you can make:
- Sit on a birth ball: Instead of slouching on the couch, try sitting on an exercise or birth ball. It naturally encourages an upright, forward-leaning posture that opens the pelvis.
- Use a wedge cushion: Place a firm, wedge-shaped cushion in your car or on your office chair to keep your hips elevated.
- Avoid deep, reclining chairs: Try to limit time spent leaning far back in soft couches, as this posture can encourage the baby to settle into a posterior position.
By making your body a more comfortable place for the baby to be in an anterior position, you are proactively setting the stage for a smoother labor and reducing the chances of a baby born face up with complications.
Gentle Exercises for Pelvic Balance
Beyond your daily posture, certain exercises can actively promote pelvic balance and help your baby find a great position. These movements are gentle and focus on creating space, not on intense physical exertion. Programs like Spinning Babies® offer a fantastic framework for understanding this kind of body balancing.
Some of the most effective and accessible exercises include:
- Pelvic Tilts: While on your hands and knees (all fours), gently rock your pelvis back and forth. This simple movement, often called "cat-cow" in yoga, helps loosen the lower back and encourages your baby to shift away from your spine.
- Forward-Leaning Inversion: Briefly inverting your body (with proper guidance and support) helps to untwist the ligaments supporting the uterus, giving your baby a chance to reposition. This should only be done for short periods, about 30 seconds at a time.
- Side-Lying Release: This is a partner-assisted stretch that helps release tension in the pelvic floor and surrounding muscles, which can create more room for your baby to navigate.
These practices aren't a guarantee, but they are empowering ways to work with your body. They help you connect with your pregnancy and play a proactive part in preparing for your birth.
The Role of Chiropractic Care
Sometimes, old postural habits or past injuries can lead to misalignments in the pelvis that are difficult to correct with exercise alone. This is where specialized prenatal chiropractic care can be a game-changer. A chiropractor trained in prenatal techniques can help restore proper balance and function to your pelvis.
One of the most well-known approaches is the Webster Technique. This is a specific chiropractic analysis and adjustment focused on reducing sacral misalignment and sacroiliac joint dysfunction. In short, its goal is to improve the neuro-biomechanical function of the pelvis. To understand how this works in detail, you can learn more about what the Webster Technique is and how it supports a healthier pregnancy.
By ensuring your pelvis is properly aligned, you create the best possible environment for your baby to move into that optimal head-down, face-down position before labor begins. This proactive care can be a key part of avoiding the challenges that come with a baby born face up.
Your Top Questions About Face Up Births
When you’re preparing for labor, hearing a term like “sunny side up” can feel a little confusing. Getting clear, straightforward answers is the best way to trade that anxiety for confidence. We've gathered the most common questions we hear from parents-to-be about the occiput posterior (OP) position to give you a quick, handy guide.
Think of this as a reference to reinforce what you've already learned and to keep on hand as you get ready for your big day.
What Causes a Baby to Be in the Face Up Position?
This is a really common question, and the honest answer is that sometimes we just don't know. A baby might settle into a face-up position simply because that’s where they got comfortable. That said, there are a few things that can influence a baby's final position before labor kicks off.
Some of these contributing factors include:
- Your Pelvic Shape: The unique anatomy of your pelvis can play a role. A more narrow or "android-shaped" pelvis might make it a bit easier for a baby to settle with their back against yours.
- Previous Pregnancies: If you've had babies before, your abdominal and uterine muscles might be more relaxed. This can give your little one more room to move around and settle into a less-than-ideal spot.
- Modern Lifestyles: We spend a lot of time sitting these days—in cars, on couches, at desks. Reclining positions can tilt the pelvis backward, which may encourage a baby to turn their back toward your back.
Often, it's a mix of these factors, or sometimes none of them at all. The most important thing to remember is that it's rarely something a mother did or didn't do.
Can I Still Have a Vaginal Birth if My Baby Is Face Up?
Yes, you absolutely can. If you take away just one thing, let it be this. A face-up position is not an automatic ticket to a C-section. In reality, many women successfully deliver their babies vaginally, even when they stay in the OP position for the entire labor.
A huge percentage of babies who start labor face up will actually rotate into the best possible anterior position all on their own as contractions do their work. For those who don't, labor might be longer and feel more intense, but a vaginal birth is still a very common and achievable outcome. Your birth team has a lot of strategies to help you and your baby get there safely.
How Will I Know if My Baby Is Face Up During Labor?
Your doctor or midwife can figure this out in a few ways. They can often get a good sense of your baby's position just by feeling your abdomen, a technique known as Leopold's maneuvers. During a cervical check, they can also feel for the baby's fontanelles (the soft spots on their head) to confirm which way they're facing.
For many moms, though, the most telling sign is the experience of "back labor." This isn't just a little ache; it's an intense, persistent pain or pressure in the lower back. It's caused by the baby's skull pressing directly against the spine, and it often continues even between contractions.
If there's any uncertainty, an ultrasound can give a clear and immediate picture of your baby’s exact position at any point during labor.
Are There Long-Term Health Issues for Babies Born Face Up?
For the overwhelming majority of babies, the answer is no. Complications like facial bruising, a temporarily cone-shaped head, or slightly lower initial Apgar scores are almost always temporary. These things usually resolve on their own or with standard newborn care within a few hours to a few days.
Long-term problems are incredibly rare and are usually linked to a particularly difficult delivery process itself, not just the baby's position. Your medical team's top priority is to monitor you and your baby closely to prevent these stressful situations and ensure a safe outcome for both of you. This is why proactive management of a face-up labor is so important—it's all about minimizing those risks.
At First Steps Chiropractic, we are dedicated to supporting you through every stage of your pregnancy and beyond. Our prenatal chiropractic care, including the Webster Technique, focuses on creating optimal pelvic alignment to help encourage your baby into the best possible position for birth. Learn more and book a complimentary consultation with our team at firststepschiropractic.com.

