If you’ve ever noticed your child seems a bit ‘floppier’ than their friends or has a tough time with motor skills, you’re not alone. What you might be seeing is low muscle tone, also known as hypotonia. It’s one of the most common physical traits we see in autistic children, often noticeable right from infancy.
This connection isn’t just a coincidence. It's a key clue into how your child's nervous system is uniquely wired and working.
Decoding the Link Between Low Muscle Tone and Autism
To understand the link between low muscle tone and autism, it helps to stop seeing them as separate issues. Instead, think of hypotonia as a direct, physical expression of a child's unique neurodevelopment. It’s a signpost pointing to the intricate relationship between their brain and body.
Think of the nervous system as the body's electrical grid, and the muscles are all the lightbulbs in the house. For a lightbulb to have a steady, ready glow, it needs a consistent and reliable flow of electricity. In a child with hypotonia, the signals from the brain and nerves that tell muscles to maintain a certain level of resting tension are often inconsistent or weaker.
This doesn't mean the muscles themselves are weak. It’s about their baseline "readiness." A child with low tone has to work much harder to generate the power needed for movement—everything from sitting up straight to holding a pencil becomes a bigger effort.
This neurological connection is why hypotonia is so widespread in the autism community. Some studies suggest that around 50% of children on the autism spectrum also have low muscle tone, which is a far higher rate than you’d see in the general population.
Recognizing this link is crucial for a few big reasons:
- It offers early clues: Hypotonia can be one of the very first observable signs that might prompt a deeper developmental evaluation.
- It explains related challenges: Many motor skill delays, posture issues, and even feeding difficulties in autism are directly tied to underlying low tone.
- It guides effective support: When we understand the neurological roots, we can seek out comprehensive care that addresses the whole child, not just one symptom.
This guide is your starting point for exploring how your child’s body and brain work together. As we dig deeper, you can also learn more about holistic approaches to autism care in our detailed article on the topic. This knowledge is power—it empowers you to find the best support and help your child truly thrive.
What Exactly Is Hypotonia

When you hear the term “low muscle tone,” it’s easy to jump to the wrong conclusion. The clinical term is hypotonia, but it has nothing to do with muscle weakness. Instead, it’s all about the baseline tension a muscle holds when it's at rest.
Think of your child’s muscles like rubber bands. A typical muscle has a certain amount of tension even when it's not being used, like a rubber band that’s already pulled just a little bit taut, ready to spring into action.
But for a child with hypotonia, those rubber bands are looser—almost slack. This means it takes a lot more effort, both mentally and physically, just to “tighten up” and get a movement started.
A Neurological Origin
This next part is really important: hypotonia isn't a problem with the muscles themselves. The issue starts in the central nervous system—the brain, spinal cord, and nerves that act as the body’s command center.
This system is supposed to send a constant, quiet stream of signals to the muscles to keep them in that state of ready tension. In kids with hypotonia, those signals are firing less efficiently or inconsistently.
The brain isn't reliably telling the muscles to stay primed and ready to go. So, while a child with hypotonia can absolutely build strong muscles, it takes a ton more energy just to get those muscles activated and coordinated.
This neurological root is a huge reason why we see such a strong link between low muscle tone and autism. Both are connected to differences in how the brain develops and communicates. The same pathways that can impact social skills and sensory processing are often the ones influencing motor control, too.
The Spectrum of Hypotonia
Hypotonia isn't a one-size-fits-all diagnosis. It exists on a wide spectrum, and its effect can look very different from one child to the next. Understanding this range helps you see where your own child might fit.
- Mild Hypotonia: This can be subtle. You might notice your child seems a bit clumsy, slumps when they sit, or just gets worn out faster than their friends during playtime.
- Moderate Hypotonia: Here, the signs are more obvious. You might see delays in motor milestones like sitting up, crawling, or walking. Many kids with moderate hypotonia prefer "W-sitting" because it gives them a wider, more stable base to sit on.
- Significant Hypotonia: In more pronounced cases, a baby might feel "floppy" or like a rag doll when you hold them. This can affect everything from holding their head up as an infant to challenges with feeding and speaking because of poor oral-motor tone.
Research backs up what we see in practice: hypotonia is a key early sign in many children later diagnosed with autism. One major study that followed 2,905 newborns found that 32.3% showed hypotonia between 0-5 months old. This was a strong predictor of later developmental hurdles, including significantly delayed walking. You can read the full study on infant hypotonia and developmental outcomes here.
Getting a handle on the fact that hypotonia is about neurological readiness, not strength, is the first step. It reframes the entire conversation and sets the stage for figuring out why it's so connected to autism and what real, whole-child support actually looks like.
Why Low Muscle Tone Is So Common in Autism
To really get to the bottom of why low muscle tone and autism go hand-in-hand so often, we have to look past the muscles themselves. This isn't just a coincidence; it's a connection that stems from shared roots in neurodevelopment. Both conditions often arise from differences in how the brain gets wired up and how it talks to the rest of the body.
Imagine the brain is an air traffic control tower, and the muscles are all the planes waiting on the runway. For a plane to be ready for takeoff at a moment's notice, it needs constant, clear instructions from the tower. For many autistic kids, that communication line has a bit of static, scrambling the signals that tell the muscles to stay in that baseline state of readiness.
This communication hiccup means the signals aren’t just weaker, but often inconsistent. That's a big reason why a child with hypotonia has to pour so much more effort into starting and maintaining every single movement.
The Brain-Body Disconnect
At the very core of this challenge are the parts of the brain in charge of motor control and coordination. One of the biggest players here is the cerebellum, tucked away at the back of the brain. The cerebellum is like the body's master control center for fine-tuning movement, balance, and posture.
In many autistic individuals, the cerebellum develops and functions a little differently. This can directly interfere with that constant feedback loop between the brain and muscles, leading to lower resting muscle tone. It’s like a world-class orchestra conductor trying to lead the musicians with a slight audio delay—the timing and intensity of the instructions are just a fraction off.
It’s estimated that around 50% of children on the autism spectrum also have hypotonia. This incredibly high number makes it clear that motor challenges aren't some separate, unrelated issue—they're often a core part of the autism profile.
This link helps explain why things like poor posture, frequent clumsiness, or trouble with motor planning (dyspraxia) are so common. These aren't just isolated physical quirks; they're the direct result of the child's unique neurological makeup.
A Closer Look at the Neuromuscular Junction
The communication breakdown can happen at an even smaller, more microscopic level. Cutting-edge research is now zooming in on the neuromuscular junction (NMJ). This is the exact spot where the nerve endings from the brain connect with the muscle fibers. Think of it as the final handshake that passes the "it's time to move" command from nerve to muscle.
It's truly remarkable that about half of kids with ASD also deal with this kind of hypotonia, sometimes being described as "floppy babies" in infancy. New studies are pointing right at the neuromuscular junction as a potential source of the problem. Early research on genetic autism models has found that these NMJs can be fragmented and poorly connected, which compromises the signal and creates a direct link between genetic factors and physical muscle weakness. To dive deeper into this fascinating science, you can explore the research on neuromuscular mechanisms in autism.
This is a huge step forward. It gives us a tangible, biological link between the genetic blueprints of autism and the real-world physical experience of low muscle tone. It helps us see that for so many children, the issue isn't a lack of effort but the integrity of the connection itself. This understanding shifts the focus from just trying to strengthen muscles to supporting the entire nervous system.
How to Recognize the Signs of Hypotonia in Your Child
Spotting the signs of low muscle tone is the first real step toward getting your child the support they need. These clues can be subtle, often blending into a child's unique developmental timeline, but knowing exactly what to look for can make a world of difference.
We’ll break down the common indicators you might see at different ages, helping you connect the dots between what you're observing at home and the underlying issue of hypotonia.
Indicators in Infants
For infants, one of the most classic descriptions parents use is that their baby feels "floppy" or like a "rag doll" when they're picked up. Instead of that firm, curled-up posture you expect in a newborn, their limbs might hang loosely. This isn't a sign of weakness, but a direct reflection of their muscles not holding that baseline tension at rest.
This can directly impact early functions that we often take for granted. An infant with hypotonia might struggle with head control, have a noticeably weak cry, or have a tough time latching during breastfeeding or bottle-feeding because the muscles in their jaw and face are also affected.
Common Signs in Toddlers
As children move into the toddler years, the signs of low muscle tone often become much more obvious through their movement and posture. Delays in hitting those major physical milestones are a huge tell.
Skills like sitting, crawling, and walking require a foundation of core strength and stability, which can be a real challenge for a child with hypotonia. For a deeper look at these important stages, check out our guide on gross motor development.
Keep an eye out for these specific patterns in your toddler:
- Delayed Milestones: They might be late to sit up on their own, crawl, pull to a stand, or take those first wobbly steps.
- "W-Sitting": You may notice your child often sits on the floor with their knees bent and legs splayed out in a 'W' shape. This position creates a wider, more stable base that demands less core muscle activation to stay upright.
- Clumsiness and Frequent Falls: A toddler with hypotonia might seem more uncoordinated than their peers, often tripping over their own feet or bumping into furniture.
- Preference for Quiet Play: They might consistently choose sitting activities over more active play like running or climbing simply because it's less physically demanding.
Indicators in School-Aged Children
Once a child reaches school age, the demands on their motor skills ramp up significantly. Here, the signs of hypotonia can show up in ways that affect both their schoolwork and their social life. The constant effort needed just to hold their body up can be draining, leaving little energy for learning and playing.
You might notice these challenges at home, or you might start getting feedback from teachers.
It's so important to remember that low muscle tone is tiring. A child who slumps at their desk isn't being lazy; their body is working overtime just to fight gravity. This constant physical effort can drain the mental energy they need for schoolwork.
Here are some common signs in older kids:
- Poor Posture: You'll see a lot of slouching, leaning their head on their hands at a desk, or frequently sliding down in their chair.
- Messy Handwriting: Difficulty with fine motor control can lead to large, poorly formed letters and a weak grip on the pencil. For them, writing can be a slow and frustrating task.
- Trouble with Self-Care: Skills like buttoning a shirt, zipping a jacket, or tying shoelaces may remain a struggle long after their peers have figured them out.
- Low Endurance: They might tire out quickly in gym class, complain about walking long distances, or avoid active games on the playground.
To help you see how these signs evolve, here’s a quick summary of what to watch for at each stage.
Developmental Signs of Hypotonia by Age Group
| Age Group | Gross Motor Signs | Fine Motor & Oral Motor Signs | Postural & Endurance Signs |
|---|---|---|---|
| Infants | "Floppy" body, poor head control, difficulty pushing up on arms | Weak suck, difficulty latching, quiet cry or coo | Feels like a "rag doll" when held, slips through hands when lifted |
| Toddlers | Delayed sitting, crawling, and walking; frequent falls; clumsiness | Difficulty using utensils, trouble with stacking blocks | "W-sitting," leans on furniture for support, tires quickly during play |
| School-Aged Children | Awkward running or jumping, avoids sports and physical games | Messy handwriting, weak pencil grasp, struggles with buttons/zippers | Slouches in chair, props head up with hands, complains of being tired |
Spotting these signs isn't about finding a label for your child. It's about understanding the "why" behind their struggles so you can become their most effective advocate.
When you can pinpoint these specific challenges, you're in a much better position to start a meaningful conversation with healthcare providers and find the strategies that will truly help your child thrive.
Therapies That Build Strength and Confidence
Once you start seeing the signs of hypotonia, the next step is putting together the right team to support your child. The goal isn't to "fix" low muscle tone but to build strength, function, and resilience so your child can navigate their world with genuine confidence. A collaborative team of therapists can create a powerful plan that addresses the connection between low muscle tone and autism from every angle.
Think of this team as a group of specialized coaches, each one focused on a different part of your child's development. They all work together, turning therapeutic exercises into real, tangible achievements that boost your child’s self-esteem.
Physical Therapy for Gross Motor Skills
A Physical Therapist (PT) is usually the first person you'll see for hypotonia. Their main focus is on gross motor skills—those big movements that use the arms, legs, and core. A PT is like a movement coach, helping your child build the foundational strength they need to run, jump, climb, and stay balanced.
PT sessions almost always look like playtime, which is key to keeping kids motivated and engaged. Your child won’t be just "doing exercises"; they'll be tackling obstacle courses, walking on balance beams like a gymnast, or bouncing on giant therapy balls. These fun activities are carefully designed to:
- Build core strength for better posture and stability.
- Improve balance and coordination to cut down on clumsiness and falls.
- Increase endurance so they can keep up with their friends on the playground.
Ultimately, physical therapy is all about making movement more efficient and less exhausting. This frees up your child to jump into all the active parts of being a kid.
Occupational Therapy for Daily Life Skills
While a PT works on the big movements, an Occupational Therapist (OT) zooms in on the fine motor skills and sensory processing needed for the everyday "jobs" of childhood. An OT’s world covers everything from holding a pencil and buttoning a shirt to making sense of all the sensory information coming in from the world around them.
OT is where the rubber meets the road, helping translate physical abilities into practical, day-to-day skills. Your OT will work on things like:
- Fine Motor Control: Strengthening hand muscles by playing with therapeutic putty, stringing beads, or working on puzzles.
- Self-Care Tasks: Practicing skills like using a fork, zipping a jacket, or tying shoes to build independence.
- Sensory Regulation: Developing strategies to help your child process sensory input in a more organized way, which has a direct impact on their motor control.
Occupational therapy helps close the gap between what a child can do physically and what they need to do to thrive at school and at home. It’s all about building functional independence, one small victory at a time.
This infographic does a great job of summarizing some of the key signs of hypotonia that these therapies target across different age groups.
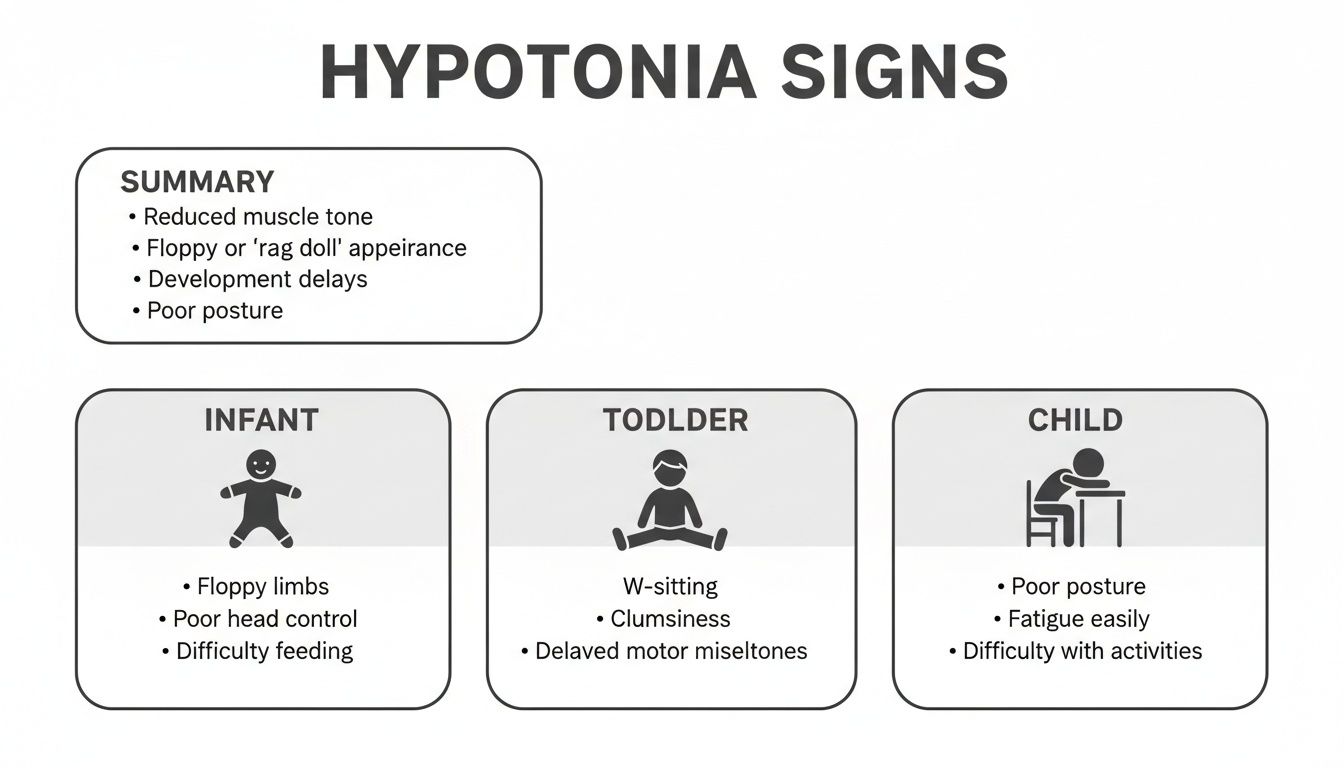
As you can see, hypotonia looks different as a child grows—from that "rag doll" feel in infancy to slumping at a school desk. This is why ongoing, adaptive therapy is so important.
Speech Therapy for Oral-Motor Challenges
Low muscle tone doesn’t just affect the limbs and core; it can also impact the small, intricate muscles in the face, jaw, and tongue. When that happens, a Speech-Language Pathologist (SLP) becomes an essential part of the team. Weak oral-motor muscles can cause real trouble with both speaking clearly and eating safely.
An SLP works to strengthen these muscles through targeted exercises that might involve blowing bubbles, practicing specific tongue movements, or using chewy tubes. This specialized work can lead to clearer speech and make mealtimes a much less stressful experience. For many autistic children, low muscle tone is a direct cause of feeding issues, making the SLP’s role absolutely critical.
A 2021 study of over 1,182 children with ASD found high rates of conditions linked to low tone, including 206 with developmental coordination disorder and 155 with muscle disorders. What's really telling is that 75 of these children had feeding disorders directly tied to their oral-motor challenges, highlighting just how vital this therapeutic support is. You can read more about these findings on the connection between ASD and motor impairments here.
Together, PT, OT, and SLP form a powerful trio of support that addresses the whole child. By working in sync, they ensure that every piece of your child’s development—from walking and writing to talking and eating—gets the attention it deserves.
Bringing Therapy Home with Everyday Activities

The progress your child makes in physical or occupational therapy doesn't have to stop when you leave the office. In fact, some of the most powerful and lasting gains happen right at home, woven seamlessly into your everyday life.
By making a few simple, intentional tweaks, you can turn your living room, backyard, and even the dinner table into a therapeutic playground. These small, consistent efforts are what truly lock in the skills they learn, transforming muscle-building from a chore into just another part of the day.
Creating a Supportive Home Environment
You can make a huge difference in your child's stability and posture just by making a few adjustments to their physical space. The idea is to provide "passive support" that encourages better body awareness without them having to constantly think about it. This frees up so much of their energy to focus on playing and learning instead of just fighting gravity.
Think about the places your child spends the most time. A few small changes can have a massive impact:
- Wobble Cushions: An inflatable wobble cushion on their chair at the dinner table or homework desk is a game-changer. It subtly engages their core muscles to keep them stable—they're getting a mini-workout without even noticing.
- Non-Slip Surfaces: A grippy bath mat in the tub or some non-slip socks on hardwood floors can boost their confidence immensely. When they feel more secure, they're less afraid of falling and more willing to move.
- Proper Seating: Check to make sure their feet can rest flat on the floor (or a stool) when they're sitting. This simple fix creates a stable base of support that makes it so much easier to sit up straight.
Think of these little environmental tweaks as gentle scaffolding. They give your child’s body the support it needs to find better alignment, which reduces fatigue and helps them participate more fully in whatever is going on.
Play-Based Exercises That Build Strength
Let's be honest—the best exercises for a kid are the ones that don't feel like exercise at all. When you tap into their natural desire to play, you can target key muscle groups in a way that feels fun and motivating. Your goal is to find activities that challenge their core strength, balance, and hand muscles.
These games are fantastic for building that crucial foundational strength:
- Animal Walks: Turn your hallway into a zoo! Bear crawls, frog jumps, and crab walks are incredibly effective for building strength in the core, shoulders, and hips.
- Play-Doh and Modeling Clay: All that squeezing, rolling, and pinching is a super fun way to strengthen the small muscles in the hands and fingers. This is essential for practical skills like buttoning a shirt or holding a pencil.
- Heavy Work Activities: Get your child involved in tasks that require some pushing or pulling. This could be helping you carry in a (light) bag of groceries, pushing a toy lawnmower, or pulling a wagon filled with their favorite stuffed animals.
- Obstacle Courses: Use pillows, couch cushions, and blankets to build an awesome indoor obstacle course. This encourages all the good stuff—crawling, climbing, and balancing—in a playful, low-pressure way.
Many of these activities also provide wonderful sensory input. If you want to learn more about how movement and sensory experiences are connected, check out our guide on sensory processing disorder therapy.
Adapting Daily Routines for Success
You can also embed these supportive activities right into your existing daily schedule. This approach ensures your child gets consistent practice without carving out extra "therapy time" from an already packed day.
Look for those little moments where you can adapt a task to help their development:
- Dressing: Let them practice with oversized buttons and zippers on their own clothes or on a special dressing toy to build those fine motor skills.
- Mealtimes: Low muscle tone often affects the jaw, making chewing tiring. Offer foods with different textures, like crunchy carrot sticks or chewy dried fruit, to give those oral motor muscles a good workout.
- Writing and Drawing: Use chunky crayons or triangular pencil grips. They provide better control and help reduce hand fatigue, making creative time much more enjoyable.
By weaving these strategies into your home life, you become a central part of your child’s care team. It's these small, consistent efforts that add up, reinforcing their progress and empowering them with the strength they need to thrive.
Your Questions Answered
When you’re navigating the world of autism and hypotonia, questions are going to come up. It's completely normal. Getting clear answers is one of the best ways to feel empowered, so let’s walk through some of the most common things we hear from parents just like you.
Can My Child's Low Muscle Tone Actually Get Better?
Yes, absolutely. While hypotonia itself is a neurological state that might not completely go away, the functional impact it has on your child's life can improve dramatically. The real goal isn't to "cure" the tone, but to build so much strength and coordination around it that it no longer holds them back.
With consistent Physical and Occupational Therapy, kids build real, functional muscle strength, endurance, and motor control. This allows them to compensate for that lower resting tone, so they can keep up on the playground and participate in all the activities they enjoy, even if they get tired a bit faster than their peers.
Is Low Muscle Tone Just Another Name for Muscle Weakness?
This is a fantastic question and a super common point of confusion. They aren't the same thing, and knowing the difference is key.
Low muscle tone (hypotonia) is about the amount of tension in a muscle when it's at rest. It’s an unconscious "readiness" signal managed by the brain. Muscle strength, on the other hand, is the power you generate when you consciously decide to contract a muscle.
A child with low tone can still become incredibly strong. The challenge is that their muscles start from a "looser" baseline, so it takes more effort for their brain and body to get them fired up and ready for action. This is often why they might seem weak or get fatigued easily.
How Do We Get a Formal Diagnosis for Hypotonia?
The first step is always a conversation. Bring up your observations and concerns with your child's pediatrician. They'll likely do an initial physical exam and, from there, refer you to a specialist for a deeper dive.
Typically, the diagnostic team will include:
- A pediatric neurologist or developmental pediatrician: They'll conduct a more in-depth assessment to figure out what might be causing the low tone.
- A Physical or Occupational Therapist: They use standardized tests to measure motor skills, reflexes, and the degree of hypotonia. This not only confirms the diagnosis but also gives them the information needed to build the perfect therapy plan for your child.
Are There Special Diets or Supplements That Can Help?
While there's no magic pill or diet that can "fix" hypotonia, great nutrition is a huge piece of the puzzle. A well-balanced diet rich in protein provides the essential building blocks your child needs to develop the muscles they're working so hard to strengthen in therapy.
It's really important to talk with your child's doctor or a registered dietitian before starting any supplements. They can check for any nutritional gaps and give you safe, personalized advice that truly supports your child's overall health and development.
At First Steps Chiropractic, we work to improve that all-important brain-body communication, supporting your child’s development from the inside out. If you're looking for a way to complement your child’s current therapies by enhancing nervous system function, we'd love to talk. You can book a complimentary consultation with our team to learn more. Visit us at https://firststepschiropractic.com.

