One second, you feel perfectly fine. The next, your heart is pounding and your vision goes blurry just from standing up. For those living with Postural Orthostatic Tachycardia Syndrome (POTS), this confusing and disorienting experience is a daily reality.
The key to understanding why this happens often lies deep within the nervous system—specifically, with the pots vagus nerve connection. When the vagus nerve isn't functioning correctly, it can throw the body's automatic processes into chaos, leading directly to the hallmark symptoms of POTS.
The Conductor and The Chaos
Think of your body’s autonomic nervous system (ANS) as a finely tuned orchestra. It’s the part of your nervous system that works silently in the background, conducting essential functions like your heart rate, blood pressure, and digestion without you ever having to think about it. It keeps everything in perfect harmony.
In this orchestra, the vagus nerve is the master conductor. As the longest cranial nerve in the body, it wanders from the brainstem down through your neck and into your chest and abdomen. It’s constantly sending signals back and forth between your brain and your organs, making sure every instrument plays its part at the right time.
When The Conductor Loses Control
POTS is essentially what happens when the conductor loses control of the orchestra. When you stand up, gravity naturally pulls blood down into your legs and feet. A healthy nervous system instantly responds. The conductor—your vagus nerve—signals the blood vessels in your lower body to tighten up and tells your heart to adjust its rate just slightly. This simple action pushes blood back up to your brain, keeping your blood pressure stable so you don't feel dizzy.
But for many people with POTS, the vagus nerve doesn't send these crucial signals effectively. The communication line is broken. The blood vessels don't get the message to constrict, so blood starts to pool in the lower body.
Your brain senses this sudden drop in blood supply and panics. It screams at the heart to beat much faster to try and compensate, creating the chaotic "tachycardia" that defines the condition. It’s like the conductor dropped the baton, and the percussion section started playing wildly to cover up the silence.
This communication breakdown is the central piece of the pots vagus nerve puzzle. The symptoms you feel—the racing heart, lightheadedness, brain fog, and crushing fatigue—are the direct results of this internal disorganization. Getting to the bottom of what vagus nerve function entails is the first step toward figuring out why your body is reacting this way.
Recognizing Vagus Nerve Dysfunction
The vagus nerve's influence goes far beyond just heart rate and blood pressure, which explains why POTS symptoms can be so widespread and seem completely unrelated. Since the vagus nerve is also a major player in digestion, a dysfunctional nerve can lead to a host of other common symptoms, such as:
- Nausea and Bloating: The nerve helps manage stomach acid and the movement of food through your gut.
- Difficulty Swallowing: It directly innervates muscles in your throat.
- Voice Changes: It also affects your larynx, or voice box.
When these digestive and throat-related issues show up alongside the classic POTS symptoms, it's a strong clue that vagal dysfunction is a major piece of the puzzle. Unraveling this complex relationship is absolutely crucial for finding management strategies that work. After all, you have to support the conductor if you want to bring harmony back to the orchestra.
How Vagus Nerve Dysfunction Drives POTS Symptoms
To really get a handle on how a struggling vagus nerve can cause so much chaos, we first need to talk about vagal tone. The easiest way to think about vagal tone is to see it as the "fitness level" of your body's internal braking system. When you have high vagal tone, your body is a pro at shifting quickly and smoothly from a state of high stress back to a state of calm.
Low vagal tone, on the other hand, is like driving a car with worn-out brakes. You slam your foot on the pedal when you need to slow down, but the car just keeps rolling along. In the same way, a vagus nerve with low tone can't effectively apply the brakes to the body's "fight or flight" system, leaving your stress response running wild without anything to check it.
The Breakdown in Communication
Every time you stand up, your body has to make a series of lightning-fast adjustments to keep blood flowing properly to your brain. A healthy vagus nerve coordinates this process without you ever noticing. But when vagal tone is low, the signals get scrambled, delayed, or are just too weak to do the job right.
This communication breakdown is the absolute core of the pots vagus nerve connection. The brain never gets the "all-clear" signal that blood pressure has stabilized, so it keeps shouting at the heart to pump faster and harder. This leads directly to that racing heart, shortness of breath, and dizzy feeling that define a POTS episode.
This is a great visual for understanding the central role the vagus nerve plays in that communication line between the brain's commands and the body's response in POTS.
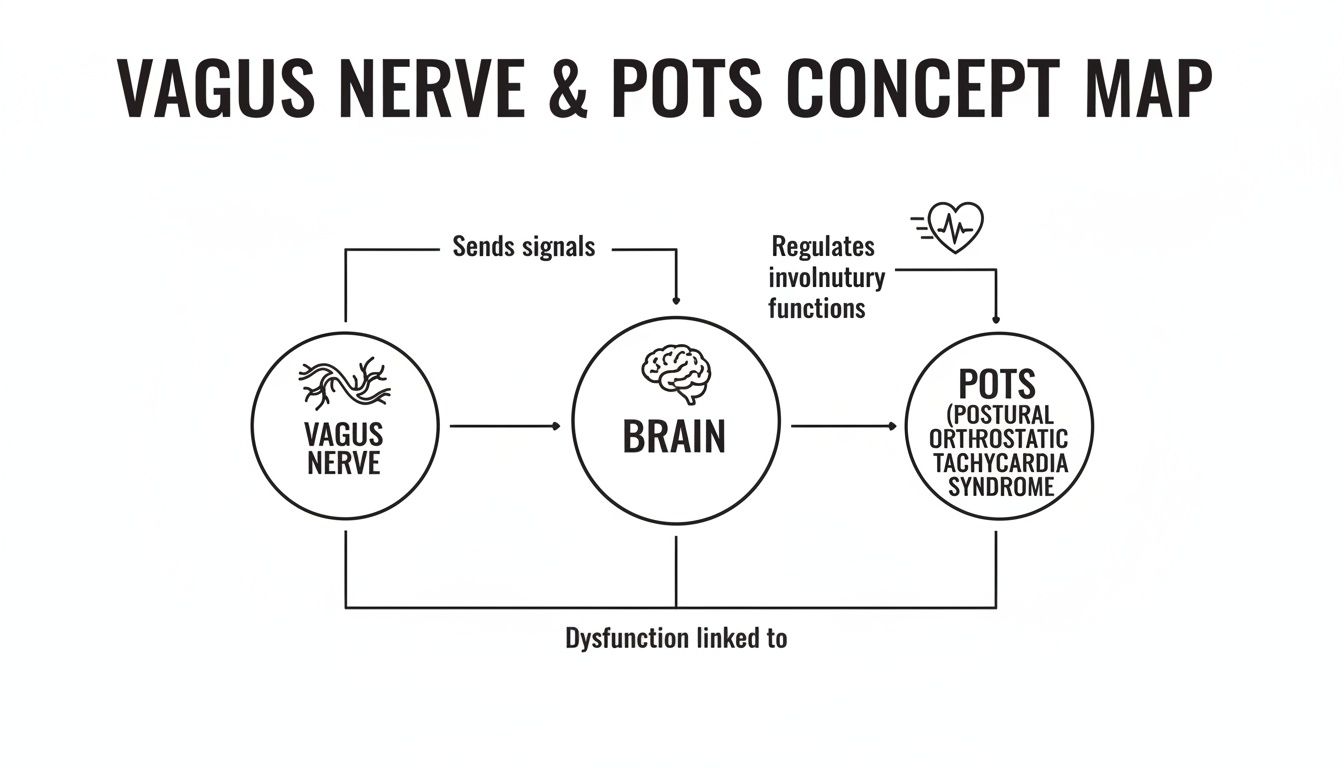
As the map shows, any disruption along that vagal pathway can trigger the dysregulated heart rate that is the hallmark of POTS.
Mapping POTS Symptoms to Vagus Nerve Dysfunction
The vagus nerve doesn't just talk to your heart; it's a massive information superhighway connecting to nearly every organ in your torso. This explains why POTS symptoms can feel so random and disconnected—they often trace back to this one critical nerve.
The table below breaks down how some of the most common POTS symptoms are directly tied to the vagus nerve's many jobs.
| POTS Symptom | Related Vagus Nerve Function | How Dysfunction Manifests |
|---|---|---|
| Tachycardia (Rapid Heart Rate) | Regulates heart rate variability (HRV) and slows heart rate. | The "brake" signal is weak, allowing the heart to race unchecked. |
| Lightheadedness/Dizziness | Manages blood pressure stabilization when changing posture. | Ineffective signaling leads to poor blood flow to the brain upon standing. |
| Brain Fog | Modulates inflammation and ensures stable blood flow to the brain. | Poor regulation can cause neuroinflammation and cognitive impairment. |
| Digestive Issues (Bloating, Nausea) | Controls gastric motility, acid secretion, and gut-brain signaling. | Sluggish digestion (gastroparesis), bloating, and nausea from poor gut function. |
| Shortness of Breath | Influences bronchial tube dilation and contraction. | A feeling of "air hunger" or difficulty taking a deep breath. |
| Difficulty Swallowing | Innervates muscles in the pharynx and larynx. | Sensations of food getting stuck or trouble initiating a swallow. |
Seeing these connections laid out makes it clear that POTS isn't just a collection of unrelated problems, but rather a systemic issue stemming from a central nervous system imbalance.
Many people with POTS suffer from significant digestive distress, which is a direct consequence of poor vagal signaling to the gut. This can show up in a few key ways:
- Gastroparesis: This literally means "stomach paralysis." It happens when the vagus nerve isn't telling the stomach muscles to contract properly, so food just sits there instead of moving into the small intestine. This is a classic cause of nausea, bloating, and feeling full almost immediately after starting to eat.
- Bloating and Constipation: The nerve also directs peristalsis—the wave-like muscle movements that push waste through your intestines. When that signaling is weak, the whole process slows to a crawl.
- Difficulty Swallowing (Dysphagia): The upper branches of the vagus nerve control the muscles in your throat, and dysfunction can make the simple act of swallowing feel difficult or uncomfortable.
"When the vagus nerve isn't firing on all cylinders, it's not just a heart rate issue; it's a full-system communication breakdown. The gut slows down, the heart speeds up, and the brain struggles to make sense of the conflicting signals, leading to brain fog."
The link between the vagus nerve and digestion isn't a new idea. The nerve's anatomy was first detailed by the physician Galen way back in the second century AD. Fast forward a few centuries, and Pavlov's famous research showed its critical role in gastric acid secretion, demonstrating that vagal stimulation could increase stomach acidity by over 50% in animal models. This discovery directly led to the development of the vagotomy—a surgery to cut the nerve—as a mainstream treatment for peptic ulcers in the 20th century. You can learn more about the history of vagus nerve research and its surprising impact on medicine.
Understanding these connections is powerful. It transforms what feels like a confusing list of random symptoms into clear signals of a nervous system imbalance, giving us a roadmap for providing targeted support.
At-Home Exercises to Strengthen Your Vagus Nerve
Taking back control of your autonomic health often starts with small, consistent actions you can take right at home. Think of these techniques as physical therapy for your nervous system. Just like you can exercise a muscle to make it stronger, you can gently stimulate and strengthen your vagus nerve over time, improving its ability to regulate your body’s automatic functions.
There’s real empowerment in knowing you have a practical toolkit to support your body. These simple, non-invasive exercises are designed to improve your vagal tone, which is absolutely crucial for managing the POTS vagus nerve connection. Small, daily efforts can add up to meaningful improvements in your overall autonomic function.
Paced Breathing: The Ultimate Reset Button
One of the most powerful and direct ways to influence your vagus nerve is simply through your breath. When you focus on a long, slow exhale, you send a powerful calming signal directly to your nervous system. It acts like a reset button for a racing heart.
This technique, often called paced or diaphragmatic breathing, physically stimulates the vagal fibers that run right through your diaphragm. So when your heart is pounding just from standing up, this simple act can help your body apply the "brakes" more effectively.
Here’s an easy way to practice:
- Inhale Slowly: Breathe in through your nose for a count of four, feeling your belly expand outward.
- Exhale Even Slower: Breathe out slowly through your mouth for a count of six or even eight, almost like you’re breathing through a straw.
- Repeat: Continue this cycle for two to five minutes. The key is to make the exhale noticeably longer than the inhale.
This deliberate slowing of your breath is a clear signal to your brain that you are safe. In response, the vagus nerve releases acetylcholine, a neurotransmitter that naturally lowers your heart rate and promotes a state of calm.
Regular practice builds this reflex, making your nervous system more resilient and better prepared to handle the postural changes that trigger POTS symptoms. The goal is to make this a natural, go-to response, not just something you do when things are already flaring up.
Activating Vagal Pathways Through Sound and Sensation
Beyond breathing, you can also physically activate the vagal pathways located in and around your throat. The vagus nerve is connected to the muscles of your larynx (voice box) and pharynx (the back of your throat), so stimulating these areas sends direct feedback right back to your brain.
These methods might seem a little unusual at first, but they are effective mechanical ways to engage the nerve directly.
- Mindful Humming or Singing: The vibrations created by humming or singing stimulate the muscles in your throat, which in turn activates the vagus nerve. Just try humming a simple tune for a few minutes each day.
- Gargling: When you gargle vigorously with water for 30-60 seconds, you activate the muscles at the very back of your throat, providing another powerful form of direct vagal stimulation.
- Cold Water Immersion: Ever splashed your face with cold water when you felt panicked? There’s a reason it works. This, or even holding an ice pack to your cheeks and neck, triggers what's known as the "mammalian diving reflex." It’s an ancient reflex that instantly slows the heart rate and redirects blood flow—a process heavily managed by the vagus nerve.
These exercises give you tangible ways to interact with and influence your own autonomic nervous system. For a deeper dive into other powerful methods, you can explore our detailed guide on how to stimulate the vagus nerve naturally.
Remember, consistency is everything. Incorporating a few of these brief exercises into your daily routine can gradually improve your baseline vagal tone, making your entire system less reactive to POTS triggers.
Foundational Lifestyle Habits for Autonomic Health

While direct exercises are a fantastic way to wake up the vagus nerve, they really shine when you build them on a solid foundation of supportive daily habits. It's all about creating an internal environment where your autonomic nervous system can find its footing and feel stable. These strategies work hand-in-hand to manage symptoms, build resilience, and strengthen the connection between the pots vagus nerve.
Think of your body as a high-performance vehicle. The vagal exercises are like fine-tuning the engine, but you won't get far without the right fuel in the tank and proper air in the tires. These foundational habits are that essential maintenance.
The Power of Salt and Hydration
For many people navigating POTS, one of the most game-changing strategies is to seriously up their fluid and salt intake. This isn't just generic wellness advice; it's a direct physiological intervention aimed at one of the core issues in POTS—low blood volume.
When you don't have enough blood circulating, your heart has to pump much faster and harder to get oxygen to your brain, especially when you stand up. Adding more salt helps your body hold onto water, which in turn boosts your total blood volume. This gives your cardiovascular system a much-needed buffer, making it far less reactive to changes in posture.
Many individuals with POTS are advised to consume 3,000-10,000 mg of sodium and at least 2-3 liters of water per day. This approach directly supports blood pressure stability and can reduce the severity of tachycardia upon standing.
This simple but powerful combination helps ensure your heart doesn't have to overcompensate so dramatically, calming the entire system. Of course, you should always chat with your doctor before making such a big change to your sodium intake.
Strategic Tools for Immediate Support
Beyond diet, certain physical tools can bring immediate relief when you feel symptoms creeping in. Think of these as reactive strategies you can deploy to help your body manage blood flow in the moment.
-
Compression Garments: Medical-grade compression stockings or an abdominal binder can make a huge difference. They work by physically squeezing the lower body, which prevents blood from pooling in your legs and abdomen and keeps more of it in the upper body where it’s needed most.
-
Physical Counter-Maneuvers: These are simple muscle contractions you can do discreetly when you feel lightheaded. Activating large muscle groups in your legs and core—like crossing your legs and squeezing, clenching your fists, or tightening your glutes—helps pump blood back up toward your heart and brain.
These tools are like having a manual override switch. They give you a way to physically help your body when its automatic systems are struggling, offering a much-needed sense of control during a flare-up.
To help you keep track of these foundational strategies, here’s a quick summary of how they fit together.
Key Lifestyle Interventions for POTS Management
This table outlines the core lifestyle changes that can provide significant relief and support for autonomic regulation.
| Intervention | Primary Goal | How It Helps |
|---|---|---|
| Increased Salt & Water | Boost Blood Volume | Helps the body retain fluid, increasing circulation and preventing a dramatic heart rate spike upon standing. |
| Compression Garments | Prevent Blood Pooling | Mechanically pushes blood from the lower body back toward the heart and brain. |
| Counter-Maneuvers | Increase Blood Pressure Quickly | Muscle contractions temporarily raise blood pressure, helping to prevent fainting or dizziness. |
| Gradual Exercise | Retrain the Cardiovascular System | Slowly improves the body's tolerance to activity and strengthens muscles that help pump blood. |
Putting these practices into place creates a stable base from which you can build further resilience.
Building Resilience Through Gradual Movement
While exercise can feel like a monumental task with POTS, a structured and gradual approach is the key to retraining your cardiovascular system. The goal isn't to push through symptoms but to slowly increase your body's tolerance to being upright and active. Recumbent exercises, like using a rowing machine or a recumbent bike, are fantastic starting points.
This kind of gentle, consistent movement helps improve muscle tone in the legs (which assists in pumping blood) and encourages the nervous system to adapt. Over time, this can lead to lasting improvements in your autonomic function.
This idea of retraining the nervous system has a surprisingly long history. The belief that nerves could heal themselves was once dismissed, but that started to change thanks to some early pioneers. Back in 1776, a surgeon named William Cumberland Cruikshank conducted experiments where he severed and then observed the reunion of the vagus nerve in animals, giving us the first real evidence of nerve regeneration. This foundational work paved the way for modern nerve repair techniques, which have seen success rates jump from 30% to over 85%. You can read more about the early history of nerve regeneration research and its incredible journey.
Exploring Clinical Treatments for Vagus Nerve Support

Sometimes, at-home exercises and lifestyle shifts just don't cut it. When you need more support, it's good to know what other options are out there. Advanced clinical interventions can offer more direct support for the pots vagus nerve connection, empowering you to have more productive conversations with your healthcare providers about the next steps.
Many of these treatments fall under the umbrella of neuromodulation. This is simply a way of using gentle electrical impulses to directly influence and help reset the nervous system’s communication lines. You can think of it as a pacemaker for your nervous system, designed to get it back into a healthier, more stable rhythm.
Understanding Vagus Nerve Stimulation (VNS)
Vagus Nerve Stimulation (VNS) is a well-established medical technology that does exactly what its name suggests—it directly stimulates the vagus nerve. It actually has a surprisingly long history, starting back in the 1880s when a neurologist developed a device to electrically stimulate the nerve to reduce seizures.
Today, VNS is a key treatment for drug-resistant epilepsy, with FDA approval since 1997 and over 100,000 devices implanted worldwide.
There are two main types of VNS you might discuss with your doctor:
- Implanted VNS: This involves a minor surgical procedure to place a small device, similar to a pacemaker, under the skin in the chest. A tiny wire runs up to the vagus nerve in the neck, where it delivers mild, pre-programmed electrical pulses.
- Transcutaneous VNS (tVNS): This is the non-invasive option that requires no surgery. A small handheld device sends electrical signals through a special earpiece that clips onto a specific part of your outer ear, stimulating a branch of the vagus nerve located there.
Both approaches are aiming for the same goal: to increase vagal tone and help regulate the autonomic nervous system. For many, tVNS offers a less invasive starting point.
Specialized Therapies for Nervous System Function
Beyond direct stimulation, other specialized therapies focus on retraining and supporting the nervous system through different means. These approaches acknowledge that conditions like POTS often stem from a complex tangle between the nervous system, the brain, and the body’s physical structure. The goal is to get to the root cause of the signaling problems rather than just chasing symptoms.
These therapies can provide a powerful framework for improving your overall autonomic health. Exploring a specialized treatment for dysautonomia can open your eyes to different clinical approaches that focus on nervous system regulation from the ground up.
By directly addressing the underlying communication breakdowns, these advanced treatments aim to help the nervous system find its way back to a more balanced and functional state, reducing the overall burden of POTS symptoms.
Having a handle on these clinical options is a crucial step in advocating for your health. While at-home strategies are a fantastic foundation, knowing about VNS and other specialized therapies allows you to explore the full spectrum of care with your medical team, opening doors to more targeted and effective support.
A Practical Guide to Navigating Your POTS Journey
Living well with POTS isn't a sprint; it's a marathon. This journey is all about understanding your body's unique signals and learning how to effectively advocate for what you need. Think of the knowledge you've gained about the POTS vagus nerve connection as your personal roadmap—but turning that map into a sustainable, day-to-day plan is what truly makes all the difference.
The very first step is to become an expert on you. One of the most powerful tools you have is consistent tracking. When you start logging your symptoms, heart rate, and lifestyle factors like diet, sleep, and daily activities, you'll begin to connect the dots and see your specific triggers and patterns emerge.
Becoming Your Own Health Advocate
Once you're armed with that data, your conversations with healthcare providers can be completely transformed. Instead of just saying, "I feel bad," you can walk in and say, "I've noticed that when I eat high-sugar foods and get less than seven hours of sleep, my morning heart rate is consistently 20 beats per minute higher when I stand up." That kind of specific detail is gold for your medical team.
Building a strong support system is just as crucial, and that starts with communicating your needs clearly and confidently.
- For Doctors: Always bring your tracked data and a list of questions to your appointments. Don't be afraid to be persistent and ask about specific strategies tied to autonomic function.
- For Family and Friends: Explain your limitations in concrete, easy-to-understand terms. For example, "Standing for more than 10 minutes can make me feel really dizzy, so I might need to sit down unexpectedly."
- For Employers or Schools: Open a conversation about reasonable accommodations. This could be something as simple as having the ability to work from a seated position or take short breaks to recline when needed.
This kind of clear communication helps everyone understand that POTS is a real, physical condition, not just a matter of stress or anxiety.
Managing the Mental and Emotional Journey
Let's be honest: living with a chronic illness is emotionally exhausting. The sheer unpredictability of POTS can stir up a lot of frustration, isolation, and anxiety. Acknowledging those feelings is a vital part of managing your overall health.
Finding your community can be a complete game-changer. Connecting with others who just get the daily realities of POTS helps shrink those feelings of isolation and opens up a space to share coping strategies and encouragement. Online support groups or local meetups can be an incredible source of validation and real-world advice.
It's also essential to build a toolkit of coping mechanisms that support your mental well-being. This might look like:
- Mindfulness and Meditation: These practices can be powerful for helping to calm an overactive, frazzled nervous system.
- Gentle Hobbies: Think about activities you can enjoy while seated, like reading, drawing, or knitting. They can provide a wonderful sense of accomplishment without triggering symptoms.
- Professional Support: Working with a therapist who has experience with chronic illness can give you invaluable tools to navigate the emotional side of this journey.
Your path with POTS is uniquely yours. By diligently tracking your symptoms, advocating for your needs, and putting your mental health first, you can build a sustainable and fulfilling life. You are the leader of your healthcare team, and every single step you take to understand and support your body is a victory.
Frequently Asked Questions About POTS and The Vagus Nerve
When you start digging into the connection between POTS and the vagus nerve, a lot of questions usually come up. We hear them all the time from families in our practice. Here are some of the most common ones, with straightforward answers to help you on your health journey.
Can Improving My Vagus Nerve Cure My POTS?
While strengthening your vagus nerve function can make a massive difference in how you feel—often dramatically reducing the severity and frequency of POTS symptoms—it's not quite a "cure." POTS is a really complex syndrome, and there are usually several different factors at play.
Think of it this way: improving your vagal tone is like upgrading your body's internal operating system. It helps everything run more smoothly and efficiently, especially how your autonomic nervous system handles daily stressors like standing up. It's an incredibly powerful management strategy, but it works best as one piece of a complete management plan you create with your healthcare team.
How Do I Know If My Vagus Nerve Is Causing My POTS Symptoms?
There isn't a single, definitive test that gives a simple "yes" or "no" answer, but there are often strong clues pointing to vagus nerve involvement. If you're dealing with significant digestive issues like gastroparesis (slowed stomach emptying), bloating, and nausea on top of the classic POTS symptoms like a racing heart and dizziness, the connection is highly likely.
Other common indicators can include:
- Trouble swallowing
- A hoarse voice or frequent voice changes
- Consistently low Heart Rate Variability (HRV) readings on a wearable device
The best way to connect the dots is to discuss this full picture of your symptoms with a knowledgeable doctor. They can help confirm if a dysfunctional POTS vagus nerve link is a primary driver behind what you're experiencing.
Are Vagus Nerve Exercises Safe For Everyone With POTS?
For the most part, yes. Gentle, non-invasive exercises like paced breathing, humming, and even mindful gargling are safe for the majority of people. The absolute key is to always start slow and listen carefully to what your body is telling you. If any exercise makes you feel worse, stop immediately.
Techniques that involve more intense physical changes, like plunging into cold water or using strong pressure-point stimulation, should be approached with more caution. It's essential to talk with your doctor or a therapist who understands dysautonomia before starting any new routine to make sure it's appropriate and safe for your specific situation.
Ultimately, these exercises are just tools to help your body regulate itself. The goal is to find what helps you feel more in control, not to push through discomfort. Building that self-awareness is a huge part of managing POTS effectively.
At First Steps Chiropractic, we specialize in getting to the root causes of nervous system dysfunction. If you're ready to see how a neurologically-focused approach can support your journey toward better autonomic health, we invite you to schedule your consultation with our team today. Find out more at https://firststepschiropractic.com.

