Managing dysautonomia often means combining beta-blockers, vasoconstrictors, and volume expanders with lifestyle tweaks—extra fluids, a bit more salt, snug compression garments, and a gradual exercise routine. Together, these strategies help steady blood pressure, boost circulating volume, and soothe an unstable autonomic system.
Quick Answer And Treatment Overview
Here’s a quick breakdown of medical and non-pharmacologic options you’ll encounter in clinical practice:
-
Beta-blockers slow the heart rate and ease symptoms like tachycardia.
-
Vasoconstrictors (for example, midodrine) lift vascular tone to counter low blood pressure.
-
Volume expanders such as fludrocortisone encourage the body to hold onto more fluid.
-
Compression garments support venous return and reduce blood pooling.
-
Exercise protocols (think recumbent cycling or tilt-table training) retrain autonomic reflexes over time.
-
Salt and fluid intake tweaks stabilize orthostatic tolerance day to day.
The infographic below shows how these approaches fit together in dysautonomia care.
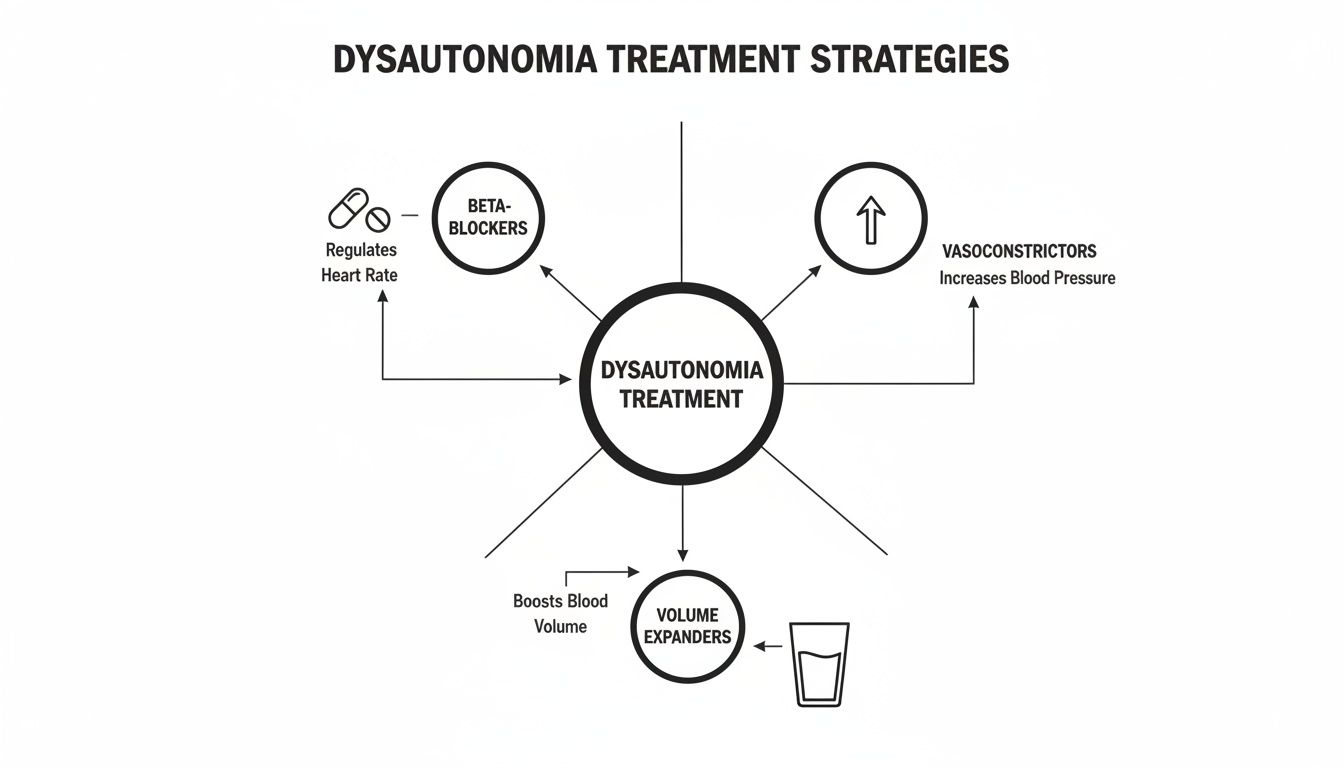
In practice, you’ll often start with beta-blockers or vasoconstrictors for immediate blood pressure support. Over weeks and months, volume expanders and lifestyle adjustments build a more stable foundation.
Overview Of Dysautonomia Treatment Options
Below is a comparison of the main treatment categories, highlighting what each aims to achieve and who tends to benefit most:
| Treatment Class | Key Interventions | Primary Goals | Typical Candidates |
|---|---|---|---|
| Beta-blockers | Propranolol, Atenolol | Heart rate control | Tachycardia-predominant |
| Vasoconstrictors | Midodrine | Increase vascular tone | Hypotension-prone |
| Volume expanders | Fludrocortisone | Boost plasma volume | Low-fluid status |
| Compression & Exercise | Garments, Tilt training | Reduce pooling, improve reflexes | Orthostatic intolerance |
This snapshot helps you see which interventions align with specific symptoms. Next, we’ll dive into each approach in greater detail. Always check in with a specialist before adjusting your treatment plan.
Understanding Pathophysiology And Diagnosis
Autonomic dysfunction feels like your body’s thermostat is on the fritz—sending mixed signals between brain and organs. It can throw blood vessel tone, gut movement, and reflexive responses completely off balance.
When reflex loops fail, standing up can trigger dizziness, fainting, and fatigue.
Affected systems include:
- Cardiovascular: low blood pressure and erratic heart rate
- Gastrointestinal: slowed motility causing bloating and nausea
- Neurological: lightheadedness and overwhelming fatigue
Core Mechanisms
Your vessels rely on rapid reflex loops to adjust when you change posture. If those loops break, rising from a chair can feel like a sudden drop on a roller coaster. Add low blood volume into the mix and perfusion to vital organs slips further—amplifying symptoms.
Diagnostic Tools
Clinicians use several key tests to pinpoint autonomic issues:
- Tilt-Table Testing tracks heart rate and blood pressure response during controlled posture shifts.
- Autonomic Reflex Screening measures sweat output, heart rate variability, and blood pressure swings.
These assessments help distinguish POTS, Orthostatic Hypotension, and other subtypes.
Early recognition can cut years off diagnostic journeys and improve care.
Delayed diagnosis often means symptoms become entrenched. Research shows an average wait of 2–7.7 years before patients receive the correct label.
Read more about diagnostic delay findings on PubMed
Check out our guide on dysautonomia and autoimmune disease for deeper context.
Specialists—neurologists, cardiologists, and autonomic experts—work together to refine the diagnosis and select the right treatment path.
Why Timing Matters
Catching dysautonomia early often means milder symptoms and a better quality of life. Letting maladaptive reflexes persist can hard-wire those faulty patterns.
Think of the autonomic system like a piano:
- Each key is a bodily response
- Stuck keys throw off the melody
- Early tuning keeps the music flowing
Primary care providers should flag red-flag symptoms—like recurrent syncope or severe orthostatic hypotension—for urgent referral. Telemedicine can bridge gaps when local experts aren’t available.
Next Steps For Patients
- Track daily readings: blood pressure, heart rate, and symptom triggers.
- Share your diary with specialists to speed up diagnosis.
- Ask about tilt-training exercises that reinforce healthy reflex loops.
- Pursue gastrointestinal motility tests if nausea and bloating persist.
- Consider skin biopsies to assess small-fiber nerve health when neuropathy is suspected.
Collaboration across specialties ensures evolving symptoms guide precise, targeted care.
Early detection lays the foundation for effective treatment for dysautonomia and better days ahead.
Analogies To Simplify
Imagine your blood volume as a water tank supplying your home. If the tank is half-empty, taps run low. Drinking more fluids and adding salt is like topping up the reservoir—maintaining steady pressure throughout the system.
Case Study Example
A 28-year-old teacher battled daily dizziness within minutes of standing. Tilt-table testing revealed a 40 bpm spike in heart rate on tilt. With dietary tweaks, compression socks, and midodrine, she saw a 70 % improvement in symptoms. This real-world success shows how an accurate diagnosis paves the way for targeted, life-changing care.
Understanding pathophysiology and diagnosis is your first milestone on the road to managing dysautonomia. Next, we’ll delve into pharmacologic therapies that directly address these core dysfunctions. Accurate, early diagnosis unlocks a smoother treatment journey ahead.
Exploring Pharmacologic Treatment Options
When the autonomic nervous system goes off balance, heart rate and blood pressure can swing unpredictably. That’s why our first stop is often cardiovascular stabilization—medications help tame a racing pulse, shore up blood volume, and ease dizziness.
Most clinicians kick off therapy with beta-blockers—propranolol or atenolol—to rein in tachycardia. We titrate slowly, targeting a resting heart rate of 60 to 80 bpm, and many patients notice they feel more grounded once their heartbeat settles.
Beta Blockers And Titration
We usually start low. Propranolol often begins at 10–20 mg twice a day, while atenolol can start at 25 mg once daily. From there, it’s a week-by-week fine-tuning.
Watching for fatigue, cold hands, or mild hypotension is key. With careful monitoring—especially for bradycardia—most people report a boost in energy and well-being as their heart rate steadies.
- Midodrine tightens blood vessels through alpha-adrenergic activation. Begin at 2.5 mg three times daily.
- Fludrocortisone expands plasma volume. A typical start is 0.1–0.2 mg each morning, paired with a high-sodium diet.
- Emerging immunotherapies, like IVIG or plasma exchange, show early promise in autoimmune‐driven dysautonomia.
Clinical trials consistently support beta-blockers as first-line agents, while midodrine and fludrocortisone team up with lifestyle changes for better symptom control. For more details, see clinical trial statistics and outcomes on PMC.
Immunotherapy In Refractory Cases
When cardiovascular agents fall short, immunotherapy can be a workaround. Intravenous immunoglobulin (IVIG) aims to reset an overactive immune response in suspected autoimmune dysautonomia.
- A standard IVIG protocol delivers 2 g/kg spread over two to five days and repeats monthly based on response.
- Common side effects include headache, chills, or mild aseptic meningitis.
Plasma exchange, which physically removes harmful antibodies, demands good vascular access and vigilant monitoring. Small trials report mixed results, so we individualize decisions carefully.
Here’s a quick comparison of the main drugs we use:
Comparison of Pharmacologic Therapies
| Medication | Class | Typical Dose | Indication |
|---|---|---|---|
| Propranolol | Beta-Blocker | 10–20 mg BID | Tachycardia Control |
| Atenolol | Beta-Blocker | 25–50 mg QD | Heart Rate Regulation |
| Midodrine | Vasoconstrictor | 2.5–10 mg TID | Orthostatic Hypotension |
| Fludrocortisone | Volume Expander | 0.1–0.2 mg QD | Plasma Volume Maintenance |
| IVIG | Immunotherapy | 2 g/kg Monthly | Autoimmune Dysautonomia |
| Plasma Exchange | Immunotherapy | 3–5 Sessions | Refractory Autoimmune Cases |
This table lays out drug classes, dosing ranges, and primary uses. It’s a handy snapshot for both clinicians and patients to match treatments to individual needs.
Titration And Monitoring
Finding the right dose takes patience. We schedule regular blood pressure and heart rate checks—lying down and standing up—to catch sudden drops. Weekly reviews let us tweak doses proactively.
Keeping a shared diary or using a simple app pays dividends. Patients log symptoms, vitals, and any new concerns. Reviewing that data at follow-ups sharpens our treatment plan and keeps everyone aligned.
- Screen for interactions—SSRIs or existing antihypertensives can shift blood pressure unexpectedly.
- Check kidney and liver function before prescribing midodrine or fludrocortisone.
- Teach patients to stand up slowly to reduce orthostatic dizziness.
- Loop in a specialist when considering immunotherapy for pediatric or complex autoimmune cases.
Blending medication with non-drug strategies—like increased fluids, compression garments, and exercise—builds resilience against core blood pressure and volume challenges.
Tailoring pharmacologic therapy to each patient’s profile ensures optimal relief and minimizes adverse effects.
Next, let’s look at how fluid optimization and compression garments work side by side with these medications to steady blood pressure and volume.
Matching Medications To Symptom Types
Dysautonomia wears different faces. In tachycardia-predominant cases, beta-blockers carry the load. When hypotension takes center stage, vasoconstrictors and volume expanders step in.
Complex or mixed presentations often call for combination therapy and expert input. Consulting an autonomic specialist becomes crucial if standard regimens miss the mark or side effects become unmanageable.
Follow-up intervals—typically every 1–3 months—allow us to reassess, adapt, and keep symptoms in check. This continuous feedback loop supports long-term stability and a better quality of life.
Engaging patients in shared decision-making fosters trust and improves adherence. Clear conversations about goals, benefits, and potential side effects pave the way to a more effective, personalized plan.
Ultimately, pharmacologic options for dysautonomia become powerful allies when paired thoughtfully with lifestyle strategies. Together, they form a comprehensive treatment framework for lasting symptom relief.
- Consult an autonomic specialist for personalized medication review and risk assessment.
- Track vital signs daily and share logs at appointments to guide titration as needed.
Applying Non Pharmacologic Strategies

Imagine your circulation as a bicycle tire—you need just the right amount of inflation to keep things running smoothly. In dysautonomia, strategic lifestyle tweaks act like pumping up that tire, boosting blood volume and steadying your pressure.
Fluid And Salt Optimization
Hydration and a bit of extra sodium can make a world of difference. Drinking enough water and aiming for 8–10 g of salt daily helps expand your circulating volume.
- Track 2–3 L of fluids with a marked reusable bottle or an app.
- Stir in electrolyte packets or sips of mineral-rich broth for added sodium and potassium.
- Keep a small shaker of salt handy—on your desk or kitchen counter—to remind you to sprinkle a bit more throughout the day.
Compression Garments And Circulation
Think of compression wear as a gentle, constant hug for your legs and abdomen. By applying 20–30 mmHg of pressure, these garments push blood back toward your heart.
Key Takeaway
Compression socks or shorts with 20–30 mmHg pressure often show symptom relief within a week.
- Opt for knee-high or waist-high garments depending on where you feel pooling.
- Slip them on during peak symptom hours—usually morning through early afternoon.
Tilt Training And Exercise
Rewiring your autonomic reflexes starts with controlled upright exposure. Small, regular sessions on a tilt table or propped on a wall can help you adapt.
- Begin at a 10° incline for two minutes once or twice a day.
- Increase the angle by 5° each week if you remain symptom-free.
- Blend in recumbent cycling or gentle yoga to strengthen leg muscles.
As you progress, these sessions become part of your daily routine. Read about how nervous-system support ties in with these strategies: Learn more about POTS and the vagus nerve.
Daily Stability Practices
Consistency builds a strong foundation. Small habits sprinkled through your day help avoid abrupt blood‐pressure shifts.
- Schedule meals and fluid breaks to match your busiest hours.
- Log symptoms, noting time, activity, and intake—patterns will emerge.
- Do quick leg pumps or gentle stretches whenever you’re on your feet for a while.
These routines mesh with medication plans, smoothing out pressure swings between doses. Regular check-ins with your provider ensure you stay on track.
Mind Body Techniques
Stress spikes can tip an already sensitive system into overdrive. Techniques that calm the nervous system are like a soothing counterweight to fight-or-flight.
- Spend five minutes each morning on diaphragmatic breathing to tame early-day adrenaline.
- Use a guided imagery app whenever tension creeps up.
Over weeks, these practices strengthen your parasympathetic “brakes,” helping you stay grounded.
Key Non Drug Takeaways
- High fluid and salt intake is like inflating a tire to maintain steady pressure.
- Compression garments deliver continuous support, especially when upright.
- Tilt training and graded exercise retrain faulty reflexes through gradual exposure.
- Symptom logs and mind-body routines reinforce stability between medication doses.
These approaches give you a practical toolkit to stabilize blood pressure and work hand-in-hand with medical therapy. With consistent use over several weeks, most patients notice measurable improvements in orthostatic tolerance and daily well-being.
Expert Insight
Integrating non-drug measures crafted like a circulatory toolkit gives patients practical control and confidence.
Integrating Autonomic Rehabilitation And Pediatric Care

Rehabilitation for dysautonomia is like tuning a piano: each key—or autonomic response—needs to hit the right note. When some keys are stuck or out of harmony, biofeedback and other techniques help restore balance.
Key Insight Retraining the autonomic nervous system can restore balance like tuning a piano to eliminate dissonance.
To get started, we rely on three pillars:
- Biofeedback Exercises let patients see heart rate or breathing patterns in real time, so they learn to self-regulate.
- Neural Modulation Methods, such as transcutaneous vagus nerve stimulation, deliver gentle electrical cues to reinforce healthy autonomic signals.
- Occupational Therapy weaves these skills into daily routines—building coordination, tolerance, and self-regulation.
Biofeedback And Modulation Techniques
Biofeedback often begins with simple, game-style activities. Imagine a character on screen that speeds up when your heart races and slows down as you calm your breathing.
Patients watch live graphs of skin conductance or pulse interval. Gradually, they learn to steer those graphs toward a steadier line.
- Interactive breathing games use fun avatars that expand on inhale and shrink on exhale.
- Heart rate variability training employs smartphone apps to guide a smooth rhythm and boost vagal tone.
- Transcutaneous electrical stimulation applies low-level currents through ear clips or pads, mimicking the body’s internal signals.
Most routines last 10–20 minutes daily. Over 4–6 weeks, many report steadier heart rates and fewer dizzy spells.
Next, occupational therapists help translate these gains into real life—adjusting classroom seating or scheduling timed breaks to prevent fatigue.
Pediatric Rehabilitation Progressions
Kids with dysautonomia often experience fatigue, headaches, or even stomach aches. Because they’re still growing, hydration and sodium need to be dialed in carefully—about 30–40 mL per kg of fluids and 2–4 g of salt daily, adjusted for age.
A typical progression looks like this:
- Begin with seated biofeedback sessions of five minutes to introduce concepts safely.
- Move on to standing breathing drills for three minutes, adding two minutes each week.
- Introduce gentle recumbent cycling or swimming: ten minutes, three times per week.
- Add proprioceptive tasks—like using weighted pencil grips—to strengthen body awareness.
Parents play a key role. They sync protocols with school routines and track symptoms at home using colorful charts. Reward systems tied to chart milestones make progress feel like play.
Engaging Families And Schools
Success hinges on teamwork. When family and school staff understand the plan, kids thrive.
- Teach caregivers simple “salt snack” recipes and fluid reminders during homework breaks.
- Work with teachers to allow standing breaks every 30 minutes and adjust seating.
- Equip staff with a clear action plan for dizziness: water spray bottles, rest areas, and emergency contacts.
- Use school-based biofeedback apps on tablets so exercises continue in class.
Regular check-ins—whether via a quick call or shared logs—keep everyone aligned.
Tip Involving siblings in breathing breaks makes rehab a family affair and boosts motivation.
Ultimately, a coordinated approach blends nervous-system “tuning” with everyday life. Consistency builds confidence—and lasting change.
Learn more about how to repair your autonomic nervous system
Recognizing Red Flags And When To Seek Specialist Care
Think of early warning signs in dysautonomia like a flickering dashboard light—ignoring them risks a breakdown. When symptoms intensify or flat-line on standard treatments, getting a specialist involved sooner can make all the difference.
For instance, recurring fainting episodes or sudden blood pressure crashes during simple tasks shouldn’t be brushed aside—they demand prompt action.
Urgent Symptoms To Watch
- Recurrent syncope episodes that interrupt daily routines
- Rapidly worsening orthostatic hypotension despite therapy
- Heart rate spikes over 30 bpm upon standing that cause dizziness
- Severe gastrointestinal dysmotility leading to dehydration
In these moments, basic measures have run their course and specialist input becomes vital to nail down an accurate diagnosis.
Case Snapshot
Take a 45-year-old patient who fainted three times in a week. Emergency tilt-table testing revealed severe autonomic failure, and an immediate neurology referral reshaped their care plan.
Rapid referral to an autonomic specialist cut recovery time by 40% in this example.
Mapping Referral Pathways
Finding the right referral route often depends on where you live and what resources you can access. Here’s a quick comparison:
| Referral Pathway | Advantages | Limitations |
|---|---|---|
| Local Specialty Clinics | In-person evaluation often same week | Rural waitlists can stretch weeks |
| Telemedicine | Connects you with experts anywhere in the country | Hinges on a stable internet connection |
| Regional Referral Centers | Multidisciplinary teams tackle complex cases | Travel costs and time off work |
When local specialists are scarce, virtual visits can bridge the gap. Remote consultations let providers review your symptom logs in real time, recommend tailored tests, and guide next steps.
Understanding COVID Impact
The pandemic did more than upend our routines—it sparked a surge in autonomic dysfunction cases worldwide. Studies suggest 67% of Long COVID patients meet criteria for dysautonomia, putting extra strain on specialty clinics.
Learn more about post-COVID autonomic challenges for treatment planning.
The COVID-19 pandemic shifted research priorities toward post-infectious autonomic dysfunction and highlighted critical gaps in care.
This spike in demand underscores why streamlined referral protocols are so important—keeping high-risk patients moving through the system without delay.
Planning Next Steps
As soon as red flags appear, primary providers can:
- Keep a detailed symptom diary—timing, triggers, and recovery.
- Order initial autonomic tests (tilt-table, heart rate variability).
- Explore telemedicine consultations with neurologists or cardiologists.
- Consider immunotherapy referrals when autoimmune dysautonomia is on the table.
Consistency in tracking and knowing when to escalate is crucial.
Jane’s Story
Jane, a 32-year-old teacher, started logging her orthostatic blood pressure at home. Her doctor shared the records with an autonomic center via telehealth, and within two weeks she began targeted immunotherapy. That collaboration slashed her diagnosis timeline from seven months to just six weeks.
Red Flags Summary And Tips
- Keep an eye on any syncope or pre-syncope events, no matter how infrequent
- Monitor heart rate and blood pressure logs daily for emerging trends
- Reach out to autonomic specialists promptly when basic measures fall short
Staying vigilant helps patients and providers navigate dysautonomia with confidence. Quick action not only speeds relief but also improves quality of life day to day.
Frequently Asked Questions
Managing dysautonomia often leaves patients wondering about the safest starting points for treatment. In my practice, three medications consistently rise to the top. Each addresses a different piece of the autonomic puzzle.
First-Line Medications
- Beta-Blockers (Propranolol): Slows the heart by blocking adrenaline’s push, easing episodes of rapid heartbeat.
- Midodrine: Tightens blood vessels to help keep you steady on your feet.
- Fludrocortisone: Boosts fluid volume in your bloodstream, making blood pressure more predictable.
High-Salt And High-Fluid Regimens
I usually recommend a 4–6 Month trial of increased salt and fluids before slowly tapering off. Marked water bottles and a salt-tracking app can turn daily goals into habits. Once you’re standing comfortably for two to three weeks in a row, it’s time to start scaling back.
Immunotherapy For Autoimmune Dysautonomia
When we suspect an autoimmune trigger, IVIG often delivers relief. The standard approach is 2 g/kg spread over three days, then monthly maintenance infusions. Side effects—headache, chills—typically ease up if the drip is slowed down.
Expert Tip: Consult an immunologist to review your treatment plan and set clear goals.
- Monitor Response by checking immunoglobulin levels and fine-tuning doses as needed.
Finding A Specialist
Not every clinic is equipped to manage complex autonomic disorders. Here’s how to connect with an expert:
- Request a neurology or cardiology referral from your primary doctor.
- Browse the Dysautonomia International Directory.
- Compare clinic approaches and read patient feedback online.
Aim for concrete targets—like cutting dizziness episodes by 50% in three months—to stay motivated. And always bring your symptom log to each visit.
Always discuss medication changes with your provider.
Contact First Steps Chiropractic for supportive nervous-system–focused care and practical tips.

