The signs and symptoms of silent reflux often disguise themselves as everyday annoyances. We’re talking about things like a persistent cough, a raspy voice, constantly clearing your throat, or that weird sensation of a lump stuck in your throat.
Unlike classic reflux, it almost never brings on the tell-tale symptom of heartburn. This is exactly what makes it so tough to pin down.
Why Silent Reflux Is So Often Misdiagnosed

When someone says "acid reflux," you probably imagine a person grabbing their chest, wincing from a fiery sensation. That intense burn is the calling card of Gastroesophageal Reflux Disease (GERD).
But there's another, sneakier version of reflux out there called Laryngopharyngeal Reflux (LPR), or silent reflux. And it plays by a completely different set of rules.
The word silent is the most important part of its name because the main alarm bell—heartburn—is almost always missing. This is why so many people, and sometimes even their doctors, chalk up the symptoms to something else entirely. That nagging cough gets blamed on seasonal allergies, a hoarse voice on a common cold, and post-nasal drip on sinus trouble.
The Mist vs. The Wave Analogy
To get a better handle on why the symptoms are so different, let’s use an analogy.
Picture classic GERD as a powerful wave of stomach acid splashing up into the lower esophagus. It’s forceful, and it causes immediate, obvious burning pain. You feel it right where it hits.
Silent reflux, on the other hand, is more like a fine, acidic mist. This isn't just acid; it's a vapor of stomach contents, including digestive enzymes like pepsin, that travels way higher up. It floats past the esophagus and settles on the delicate tissues of your throat, voice box (larynx), and even your nasal passages.
These upper airway tissues were never built to handle any level of acidity. Even tiny, brief exposures to this damaging mist can cause significant inflammation and irritation over time, leading to chronic symptoms without that classic fiery feeling of heartburn.
This subtle but constant irritation is precisely why silent reflux signs and symptoms show up in the throat and respiratory system instead of the chest.
A Common But Underrecognized Condition
Because it lacks those obvious reflux symptoms, LPR often flies under the radar for months, if not years. People can spend a long time cycling through allergy pills, inhalers, and cough syrups, finding little to no relief because they aren't treating the actual root cause.
This diagnostic merry-go-round is incredibly common, even though the condition itself is widespread. Globally, it's estimated that GERD, the umbrella category that includes silent reflux, affects about 1.03 billion people. You can dive deeper into the data by exploring the full systematic review about GERD prevalence.
Learning to spot the unique pattern of LPR is the crucial first step. Here are the most common clues that you might be dealing with something more than just a cold you can't shake:
- Constant throat clearing: A persistent "tickle" or feeling of mucus in your throat that you have to clear.
- Hoarseness or voice changes: Your voice might sound raspy, weak, or tired, and it's often worse in the morning.
- Chronic cough: A dry, nagging cough that just won't go away and doesn't seem linked to being sick.
- Globus sensation: That deeply unsettling feeling that you have a lump or a pill stuck in your throat when you swallow.
Decoding the Telltale Symptoms in Adults

In adults, the signs of silent reflux often feel like a frustrating collection of unrelated issues that just won't go away. You might find yourself bouncing between specialists—seeing an allergist for post-nasal drip or a lung doctor for a nagging cough—without ever connecting the dots back to your digestive system.
That’s because the real trouble isn't happening in your chest; it's occurring much higher up.
Unlike classic heartburn, LPR allows stomach contents to travel all the way up to the delicate tissues of your throat (pharynx), voice box (larynx), and even your sinuses. These areas simply aren't built to handle any level of stomach acid, which is why the symptoms are often so confusing and distinct from typical reflux.
This is exactly why LPR gets missed so often. The lack of obvious heartburn can be so complete that serious damage can happen without you ever feeling a thing. In fact, research shows that nearly 37% of patients with medically confirmed erosive damage to their esophagus from reflux reported no symptoms at all. You can dive into the research about symptom-free esophageal damage to learn just how common this is.
Throat and Voice Symptoms
The most common cluster of silent reflux signs and symptoms centers around the throat and voice. This is a direct result of a fine mist of stomach acid and digestive enzymes, like pepsin, making contact with your vocal cords.
Over time, this constant, low-level irritation leads to a whole host of frustrating problems:
- Persistent Hoarseness: Your voice might sound raspy or weak, especially first thing in the morning after a night of reflux.
- Chronic Throat Clearing: A nagging tickle or the feeling of thick mucus forces you to constantly clear your throat just to speak.
- Globus Sensation: This is that weird, unsettling feeling that a lump or a pill is stuck in your throat, even when it’s completely empty.
- Sore or Irritated Throat: A lingering, mild sore throat that hangs around without any other signs of sickness, like a fever.
These symptoms pop up because pepsin, a powerful digestive enzyme, gets "activated" by the acidic environment. When it lands on your throat tissue, it starts causing inflammation and cellular damage, leading to the symptoms you feel.
Respiratory and Sinus Issues
When that acidic mist travels even higher, it can wreak havoc on your entire upper respiratory system. The inflammation can easily spread into your sinuses and airways, kicking off symptoms that are very commonly mistaken for allergies or asthma.
Think of it like a chemical irritant setting off your body's defense systems. Your nasal passages start producing extra mucus to protect themselves, or your airways might tighten up in response.
This can show up as:
- A Chronic, Dry Cough: This is a hallmark sign of LPR, often getting worse after you eat or when you lie down.
- Post-Nasal Drip: The sensation of mucus constantly dripping down the back of your throat.
- Asthma-Like Symptoms: Reflux irritating the airways can trigger wheezing or shortness of breath. In some people, LPR can even make their existing asthma harder to manage.
- Recurring Sinus Infections: Chronic inflammation can block your sinus passages from draining properly, creating the perfect environment for infections to take hold.
Silent Reflux (LPR) vs. Classic GERD Key Symptom Differences
Understanding the difference between LPR and classic GERD is the key to getting a proper diagnosis. While they both stem from the same root problem—stomach contents moving the wrong way—their impact on your body is worlds apart.
The core difference lies in where the symptoms show up. GERD shouts its presence with chest pain and heartburn, while LPR whispers through persistent throat and breathing issues.
This table breaks down the key differences to help you see which condition your symptoms might be pointing toward.
| Symptom Area | Silent Reflux (LPR) | Classic GERD |
|---|---|---|
| Primary Sensation | Throat irritation, lump in throat, hoarseness | Burning chest pain (heartburn), acid taste |
| Main Location | Throat, voice box, sinuses | Lower chest, upper abdomen |
| Key Indicators | Chronic cough, constant throat clearing | Acid regurgitation, indigestion |
| Timing of Symptoms | Often present throughout the day, can be worse in the morning | Typically worse after meals or when lying down |
| Heartburn | Rare or absent | The defining, most common symptom |
Recognizing these patterns is the first step toward having a productive conversation with your doctor. If you've been fighting a chronic cough or a scratchy voice with no relief, it might be time to consider that the problem isn't starting in your throat, but much lower down.
Recognizing Silent Reflux in Infants and Children
Trying to pinpoint silent reflux in your little one can feel like you're trying to solve a puzzle with half the pieces missing. Unlike adults who can tell you they have a scratchy throat or heartburn, babies and young kids communicate entirely through their behavior. This makes the silent reflux signs and symptoms incredibly subtle and all too easy to mistake for something else.
For parents, this often becomes a frustrating and confusing journey. You have that gut feeling that something isn't right, but the signs just don't fit into a neat little box. What might look like a simple case of fussiness or colic could actually be your child’s way of telling you they’re uncomfortable from Laryngopharyngeal Reflux (LPR).
Common Signs in Infants
With the youngest patients, the clues for silent reflux often appear during or right after feeding time. A little bit of spitting up is perfectly normal—their digestive systems are brand new, after all. But with LPR in infants, it’s less about the spit-up and more about signs of irritation and pain.
Just imagine it for a second: even a tiny, invisible mist of stomach acid reaching their delicate throat can be startling and painful. This can quickly turn feeding, which should be a time of comfort and bonding, into a stressful event for both you and your baby.
Keep an eye out for these telltale behaviors:
- Arching the back during or after feedings: This is a classic sign of pain. Your baby is instinctively trying to lengthen their esophagus to get some relief from the discomfort.
- Frequent fussiness or crying: If your baby seems irritable for long stretches without a clear reason, it could very well be reflux-related pain.
- Poor feeding or feeding refusal: They might start to nurse or take a bottle, then suddenly pull away crying, or just refuse to eat altogether.
- Trouble sleeping: Lying flat can make reflux much worse, leading to frequent waking, especially if they sound congested when they're on their back.
- Poor weight gain: When feeding becomes a constant battle, they may not get the calories they need to grow at a healthy pace.
These signs can be especially tricky because they overlap so much with other common infant issues. It's no wonder parents are left wondering if they're dealing with reflux or something else entirely. For those of you navigating this uncertainty, learning to decode your baby's cries is key. You can find more insight in our guide on colic relief for newborns.
What to Look for in Older Children
As children grow, the signs of silent reflux start to resemble the adult version more, but they still get misdiagnosed all the time. A nagging cough gets blamed on seasonal allergies, and a hoarse voice is written off as the leftover effect of a common cold.
The real key is to look for chronic patterns—symptoms that just seem to hang around for weeks or even months without a clear cause. Since kids can't always connect a "sore throat" to something happening in their stomach, it’s up to parents and caregivers to spot the connection.
A child with silent reflux might never say, "my chest hurts." Instead, their body expresses the discomfort through respiratory and throat-related issues that never seem to fully resolve.
Here are some of the most common signs you might see in toddlers and school-aged children:
| Symptom Category | Specific Signs to Watch For | Why It Happens |
|---|---|---|
| Respiratory Issues | Chronic, dry cough (especially at night) Wheezing or asthma-like symptoms Recurrent croup or bronchitis |
The acidic mist irritates the airways, causing inflammation and triggering a cough reflex or airway constriction. |
| Throat & Voice | Persistent hoarseness or a raspy voice Constant need to clear the throat Complaining of a "lump" in their throat |
Stomach contents directly irritate the vocal cords and laryngeal tissues, leading to swelling and voice changes. |
| Ear & Nose | Frequent or recurring ear infections Chronic sinus congestion or post-nasal drip |
Reflux can inflame the Eustachian tube opening, trapping fluid in the middle ear and leading to infections. |
Paying close attention to these patterns is crucial. If your child seems to be constantly on antibiotics for ear infections or uses an inhaler with little to no improvement, it might be time to consider silent reflux as a possible culprit and bring it up with your pediatrician.
What Causes LPR and Who Is at Risk?
To really wrap your head around silent reflux, it helps to picture your digestive system as a highly organized one-way street. Normally, two muscular "gates," called sphincters, make sure that all traffic—meaning food and stomach acid—keeps moving in the right direction: down.
The first gate, the lower esophageal sphincter (LES), is positioned between your esophagus and stomach. A second, higher gate, the upper esophageal sphincter (UES), stands guard at the top of your esophagus, protecting your throat. When they're working as a team, they clamp down tightly to keep potent stomach contents where they belong.
But in silent reflux, one or both of these gates get a little lazy. They might weaken, relax when they shouldn't, or just not close all the way. This opens the door for a fine mist of stomach contents, including acid and digestive enzymes like pepsin, to travel upward. It sneaks past the esophagus and irritates the incredibly sensitive tissues in your throat, voice box, and even your nasal passages. This is the root cause of that nagging throat-clearing, hoarseness, and persistent cough.
Common Triggers and Risk Factors
So, what makes these protective sphincter "gates" malfunction? A lot of factors can contribute, and pinpointing them in your own life is the first real step toward getting a handle on your symptoms. Often, the culprits are tied directly to our daily habits.
Key contributors include:
- Dietary Choices: Some foods are notorious for telling the esophageal sphincters to relax. Think fatty or fried foods, chocolate, caffeine, alcohol, fizzy drinks, and highly acidic things like tomatoes or citrus.
- Lifestyle Habits: Simple things like eating too much in one sitting, having a large meal right before bed, smoking, or even wearing tight clothes can all ramp up the pressure in your abdomen, physically pushing stomach contents upward.
- Excess Body Weight: Carrying extra weight, especially around your middle, puts constant pressure on your stomach and the LES. This makes it much easier for reflux to happen.
Underlying Health Conditions and LPR
Sometimes, silent reflux isn’t just about what you ate for dinner. It can be linked to other health issues that throw off the body’s muscular or nervous system coordination, disrupting the delicate signals needed to keep those sphincter gates working properly.
It's important to remember that silent reflux doesn't always show up by itself. It can be a symptom of a bigger imbalance in the body, which just goes to show how interconnected our digestive, nervous, and even cardiovascular systems really are.
For example, conditions that slow down how quickly your stomach empties, like gastroparesis, leave acidic contents sitting around longer, creating more opportunities for them to reflux. The complex signaling needed for those sphincters to open and close at the right times is managed by your nervous system. To get a better sense of this crucial connection, you can read our guide on what is vagus nerve function.
There's also a surprising link between LPR and heart health. Research has found a significant connection between hypertension (high blood pressure) and silent reflux. A 2016 study, for instance, discovered that 15.1% of patients with hypertension also had silent GERD. The study identified abdominal obesity and unmanaged high blood pressure as key predictors. This shows how bigger, system-wide health problems can directly increase your risk for silent reflux, making a holistic view of your health absolutely essential.
How Doctors Diagnose Silent Reflux Accurately
Pinpointing silent reflux isn't as straightforward as identifying classic heartburn. Since the telltale silent reflux signs and symptoms can easily be mistaken for allergies or even a common cold, doctors have to play detective to get to the root of the problem. This requires a careful, step-by-step approach to solve the mystery behind that persistent cough or constant throat clearing.
It all starts with a simple conversation. Your doctor will want to know every detail—what you're feeling, how long it's been happening, and what seems to make it better or worse. This initial chat lays the entire groundwork for the diagnostic journey.
Starting With a Physical Exam
After you've talked through your symptoms, the next logical step is a physical exam. Usually, this is handled by an ear, nose, and throat (ENT) specialist, who will look for the physical clues that stomach contents have been making their way into your upper airway.
The go-to procedure here is a laryngoscopy. Using a tiny, flexible camera that's passed through the nose, the doctor gets a direct look at your throat and voice box (larynx). They're hunting for specific signs of LPR, including:
- Redness and swelling: Inflammation around the vocal cords is a major red flag.
- Thickened mucus: The body often produces extra mucus in an attempt to protect the irritated tissues.
- Tissue changes: Over time, chronic irritation can cause visible changes to the delicate lining of your throat.
This is a quick, in-office procedure that provides the first real evidence that your symptoms could be tied to reflux.
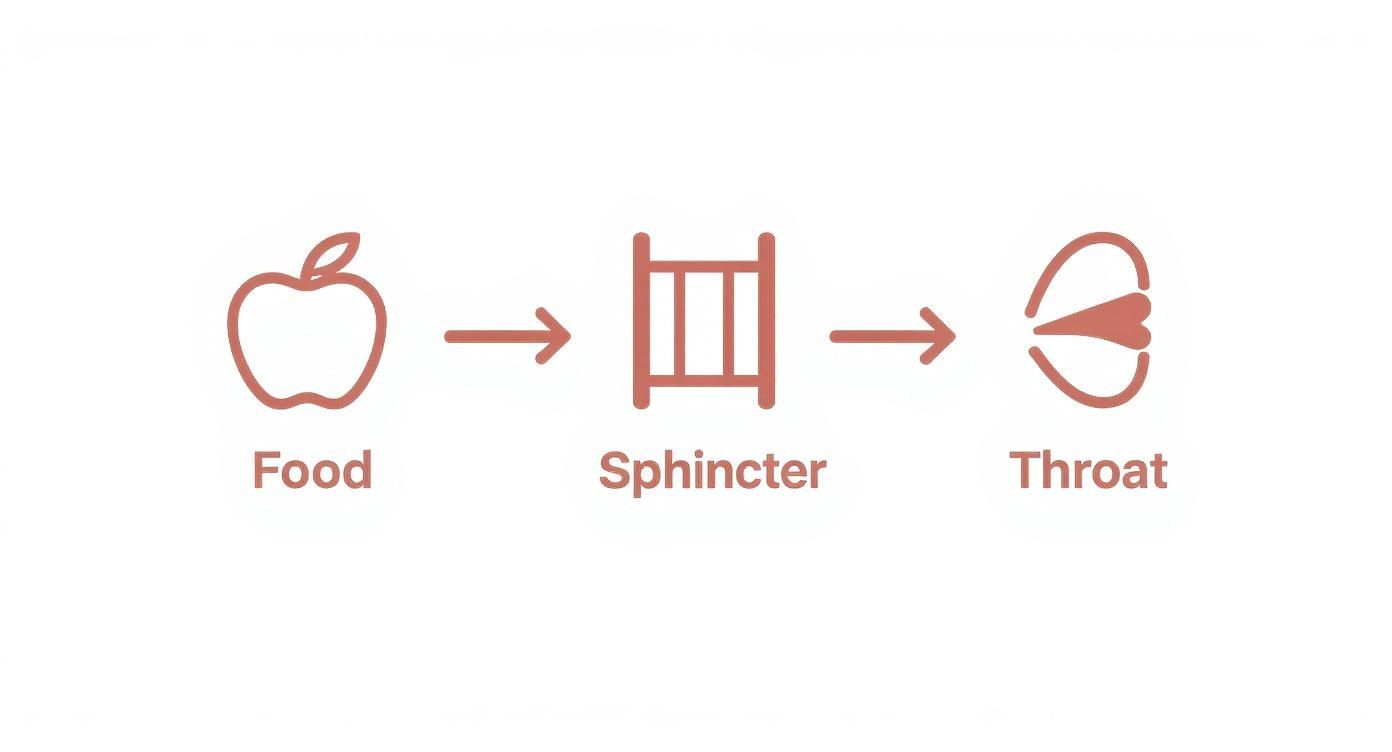
This visual helps show how a weak or malfunctioning sphincter allows acid and enzymes to travel up into the throat, leading to the kind of irritation your doctor is looking for.
Advanced Diagnostic Testing
What happens if the physical exam points strongly to LPR, but initial treatments aren't helping? Your doctor might recommend more advanced testing to get a definitive answer. These tests are designed to actually measure reflux activity in real-time.
The gold standard for a conclusive diagnosis is 24-hour pH impedance testing. For this test, a very thin, flexible tube is placed through your nose and down into the esophagus. Over a full 24-hour period, it measures both acidic and non-acidic reflux events.
This test is a game-changer because it provides hard data. It shows exactly how often stomach contents are reaching your throat and, more importantly, if those events line up with when you feel symptoms. It takes the guesswork out of the equation.
A few other tests might also be on the table:
- Barium Swallow Study: You’ll drink a chalky liquid that coats your digestive tract, allowing a radiologist to watch how you swallow on an X-ray. It's a great way to spot any structural issues that might be contributing to your reflux.
- Esophageal Manometry: This test measures the muscle contractions in your esophagus when you swallow. It’s all about checking the coordination and strength of your esophageal sphincters to see if they are doing their job properly.
Together, these diagnostic tools help your doctor build a complete picture of what's really going on inside, ensuring you get the right diagnosis and, ultimately, the most effective treatment plan.
Effective Treatment and Management Strategies for LPR

Finding lasting relief from silent reflux, or Laryngopharyngeal Reflux (LPR), is almost never about a single, quick fix. It’s more of a long game. Real success comes from a multi-layered approach that weaves together smart daily habits with the right medical support.
Think of it less like putting out a fire and more like redesigning the environment so fires can't start in the first place. This means we have to tackle the root causes—like a weak sphincter or too much stomach acid—from a few different angles. For most people, combining lifestyle tweaks, dietary changes, and medical treatments is what finally beats back those persistent silent reflux signs and symptoms.
Foundational Lifestyle and Dietary Modifications
Honestly, the most powerful tools you have for managing LPR are the changes you make in your everyday routine. These adjustments work by taking pressure off your esophageal sphincters and dialing back the amount of acid your stomach produces.
Simple, consistent changes can make a world of difference. Start by zeroing in on these high-impact habits:
- Avoid Trigger Foods: Some foods are notorious for relaxing the lower esophageal sphincter, practically opening the door for reflux. The usual suspects include caffeine, chocolate, alcohol, mint, greasy or fried foods, and anything fizzy.
- Mind Your Meal Timing: This one is huge. Stop eating at least three hours before you lie down for the night. This gives your stomach plenty of time to empty out, slashing the risk of overnight reflux.
- Elevate Your Head While Sleeping: Use a wedge pillow or put some blocks under the head of your bed to raise it by 6 to 8 inches. Gravity becomes your best friend, helping keep stomach contents right where they belong.
- Eat Smaller, More Frequent Meals: Big meals crank up the pressure inside your stomach, which can physically push acid and food upward. Go for smaller portions spread throughout the day to keep that pressure down.
These habits are all about reducing the opportunity for reflux to happen. When you do that, you give your irritated throat and vocal cords a much-needed break and a real chance to heal.
Medical Treatments for LPR
When lifestyle changes just aren't cutting it, your doctor might recommend medication. The goal here is usually to either neutralize stomach acid or, more often, to dramatically reduce how much acid your stomach makes.
Think of these medications as turning down the "acidity dial." Reflux might still occur, but the fluid that comes up is far less corrosive and damaging to the delicate tissues in your throat and voice box.
The point of medical therapy isn't just to mask the symptoms. It’s to give the inflamed tissues in your larynx and pharynx the time they need to truly heal, a process that can take weeks or even months of consistent treatment.
The most common medical options include:
- Proton Pump Inhibitors (PPIs): These are powerful medications that effectively block acid production. They are often the first line of defense for LPR and are usually taken 30-60 minutes before your first meal of the day.
- H2 Blockers: These drugs also cut down on stomach acid but are generally less potent than PPIs. Your doctor might suggest them for milder symptoms or have you take one before bed to control nighttime acid.
Complementary Approaches for Holistic Care
Beyond diet and medication, other strategies can give your body’s healing process a major boost. These complementary approaches often focus on reducing overall inflammation and improving how your digestive and nervous systems function.
Managing systemic inflammation is key, as it can make tissue irritation worse everywhere in your body, including your throat. You can learn more about practical strategies in our guide on how to reduce inflammation.
On top of that, many people find relief by addressing the mind-body connection. Stress is a well-known reflux trigger. Practices like deep breathing exercises, meditation, or even gentle yoga can help calm the nervous system, which in turn can lessen the severity of reflux episodes. Building a well-rounded plan that includes lifestyle, medical, and complementary strategies gives you the absolute best shot at finding long-term freedom from silent reflux.
Your Questions About Silent Reflux, Answered
When you're dealing with symptoms that don't quite add up, it’s natural to have a lot of questions. Silent reflux can be confusing, especially since its signs often mimic other issues. Let’s clear up some of the most common questions we hear from families.
Can Silent Reflux Go Away on Its Own?
This is a really common question, especially for parents of little ones. While it's true that some mild cases in infants might resolve as their tiny digestive systems mature, LPR in adults and older children usually needs a more proactive approach.
For most, the symptoms are chronic and can lead to bigger problems if they're just ignored. Lasting relief typically comes from a combination of consistent dietary changes, lifestyle shifts, and sometimes medical support. Simply waiting for the silent reflux signs and symptoms to fade isn't a reliable strategy for most people.
How Long Does Treatment Take to Work?
The timeline for feeling better really varies from person to person. Some people start to notice a real difference within a few weeks of sticking to diet and lifestyle adjustments.
If a doctor prescribes a medication like a Proton Pump Inhibitor (PPI), it can take 4 to 8 weeks to feel significant relief. That’s because the irritated tissues in the throat and voice box need time to heal from all that chronic inflammation.
Patience is key here. It’s all about consistency with your treatment plan. For symptoms that have been around for a long time, it might take several months of dedicated effort to feel fully back to normal.
Is Silent Reflux a Serious Condition?
While it’s not something that’s immediately life-threatening, silent reflux can absolutely become a serious issue if it’s left unmanaged over the long haul. The constant exposure of those sensitive tissues to stomach contents can cause significant problems down the line.
We’re talking about things like:
- Permanent vocal cord damage and scarring
- Recurring and severe respiratory infections
- An increased risk of certain throat cancers
Because there's no classic heartburn, it's easy to get a false sense of security. This is exactly why recognizing those "silent" signs and getting a proper diagnosis is so crucial for preventing more severe health outcomes later on.
At First Steps Chiropractic, we know that true wellness comes from getting to the root cause of your family's health challenges. If you're navigating complex symptoms like those from silent reflux, our neurologically-focused approach may offer the support you're looking for. Discover how our personalized care plans can help optimize your family's health.

