At its core, the connection between dysautonomia and autoimmune disease is a classic case of mistaken identity. The immune system, our body’s built-in security force, gets its wires crossed and begins to attack components of the autonomic nervous system. This "friendly fire" incident throws the body's autopilot system into chaos, leading to a cascade of confusing and often debilitating symptoms.
Untangling the Wires of Your Nervous System

Think of your body as a complex, high-tech building. Your immune system is the security team, constantly on patrol for intruders. Your autonomic nervous system (ANS) is the building's entire automation system—it handles everything from the air conditioning (body temperature) to the water pressure (blood pressure) without you ever having to think about it. It’s the master control panel that keeps everything running smoothly behind the scenes.
But when an autoimmune disease is in the picture, it's like the security team starts working off faulty intelligence. It begins to see the building’s own wiring—the nerves of the ANS—as a threat and launches an attack.
This assault can trigger widespread, unpredictable system failures. All of a sudden, the elevator (your heart rate) might race out of control just from standing up, or the plumbing (your digestive system) might grind to a halt. This is dysautonomia in a nutshell: a malfunction of the body’s internal wiring caused by an immune system gone rogue.
To help clarify these two distinct but related conditions, let's break them down side-by-side.
Key Concepts At a Glance: Dysautonomia vs. Autoimmune Disease
| Characteristic | Dysautonomia | Autoimmune Disease |
|---|---|---|
| Primary Target | The autonomic nervous system (ANS) | Any body tissue or organ (joints, skin, nerves, etc.) |
| Core Problem | Malfunction of "automatic" bodily functions (heart rate, digestion) | The immune system mistakenly attacks healthy cells |
| Nature of Condition | A neurological condition | An immune system condition |
| Common Symptoms | Dizziness, fatigue, rapid heart rate, digestive issues | Joint pain, skin rashes, inflammation, fatigue |
| Typical Cause | Can be primary (on its own) or secondary to another condition | An overactive and misdirected immune response |
This table shows how one (autoimmune disease) can directly cause the other (dysautonomia), creating a complex web of symptoms.
Why This Connection Matters So Much
Understanding this link is a huge step forward because it validates the experiences of countless people who feel lost between medical specialties. Their symptoms often don't fit neatly into one box, which leads to a frustrating and exhausting diagnostic journey.
Recognizing that an immune system problem can directly cause neurological symptoms is the key to connecting the dots and finding clarity.
The relationship between these conditions explains why someone might have a bewildering mix of symptoms—like joint pain from an autoimmune condition such as lupus alongside the lightheadedness and digestive issues of dysautonomia. They aren't two separate problems but different expressions of the same underlying conflict.
The Scope of Dysautonomia
Dysautonomia is far more common than most people think. It's estimated to affect 70 million people worldwide, yet it remains widely underrecognized by both the public and many in the medical community.
Among its different forms, Postural Orthostatic Tachycardia Syndrome (POTS) is one of the most well-known, impacting about 1 in every 100 teenagers. POTS has a significant gender disparity, affecting women at a 5:1 ratio compared to men, often during their younger years. You can find more details on these global health statistics from the Dysautonomia Support Network.
This intersection of dysautonomia and autoimmune disease isn't a rare coincidence; for many, it’s a critical piece of the chronic illness puzzle. By exploring this connection, we can start to map out a clearer path toward effective diagnosis, management, and a better quality of life.
Understanding Your Body's Autopilot System
Think about your body for a second. Right now, you're not consciously telling your heart to beat, your lungs to breathe, or your stomach to digest. These things just happen, running smoothly in the background like a perfectly programmed autopilot system. This incredible, silent system is your autonomic nervous system (ANS).
The ANS is the master control center for all the automatic processes that keep you alive and stable. It's constantly adjusting your heart rate, blood pressure, digestion, and body temperature without you ever having to think about it. It’s the behind-the-scenes operator making sure your internal world stays in balance, a state we call homeostasis.
But what happens when that sophisticated autopilot system starts to glitch? The result is dysautonomia. It isn't just one specific disease but rather a broad term for when the ANS malfunctions. All those automatic functions you’ve relied on your whole life suddenly become unpredictable and chaotic.
When the Internal Computer Malfunctions
Imagine the ANS as your body's internal computer, constantly taking in data from your surroundings—things like gravity when you stand up, the temperature in the room, or a stressful situation—and making instant, perfect adjustments.
Dysautonomia is like a software bug corrupting that computer. The commands it sends out become faulty. Standing up might trigger an error message that sends your heart racing, or eating a meal could cause a system crash in your digestive tract. This malfunction is often at the heart of the connection between dysautonomia and autoimmune disease, where the immune system's misdirected attack is the very thing "corrupting the software."
Because the "glitch" can show up in different ways, there are several types of dysautonomia.
- Postural Orthostatic Tachycardia Syndrome (POTS): This is one of the most common forms you’ll hear about. Picture it as a faulty gravity sensor. When you stand up, the system fails to correctly signal your heart and blood vessels to adjust, causing your heart rate to spike dramatically.
- Orthostatic Hypotension (OH): This condition causes a sharp drop in blood pressure when you stand, leading to dizziness or even fainting. It’s like a fuel pump that can't supply enough pressure when a car starts going uphill.
- Neurocardiogenic Syncope (NCS): A frequent cause of fainting, this happens when the system overreacts to a trigger, causing a sudden, steep drop in both heart rate and blood pressure.
At its core, dysautonomia is a communication breakdown. The brain isn’t getting the right signals from the body, or it’s sending out the wrong commands in response. This creates a ripple effect of problems throughout the body.
The Overlap with Other Conditions
Dysautonomia rarely shows up alone. Because the ANS has its hands in every single system in the body, its dysfunction often appears alongside other complex health issues, creating a tangled web of symptoms that can be confusing for both patients and doctors.
This isn't a coincidence. It points to a deeper, more systemic issue affecting the whole body. We see this clearly in the research. A major clinical study, for example, found that Ehlers-Danlos syndrome (a connective tissue disorder) was present in a staggering 42.9% of dysautonomia patients. Mast cell activation disorders were identified in 33.0% of patients, and various nutritional deficiencies were found in 29.6% of cases. You can dig into the specifics of these co-occurring conditions and learn more about the data linking them to dysautonomia.
Seeing the ANS as your body’s autopilot helps make sense of symptoms that might otherwise seem completely random. It’s not "all in your head"; it's a real, measurable issue with the master control system that’s supposed to keep everything running smoothly.
How Autoimmune Responses Trigger Neurological Symptoms
To really get the link between dysautonomia and autoimmune disease, we have to look at what’s happening on a microscopic level. A healthy immune system is like a well-trained security team, protecting you from outside threats like viruses. But in an autoimmune condition, that team gets confused. It starts seeing your own healthy tissues as the enemy and launches an attack—a classic case of friendly fire.
When the nervous system gets caught in the crossfire, dysautonomia is often the result. This breakdown happens in a couple of key ways, starting with the immune system creating rogue agents called autoantibodies.
The Role of Autoantibodies
Think of antibodies as your body's guided missiles, programmed to find and destroy specific invaders. In an autoimmune disease, the body starts making autoantibodies—missiles programmed with the wrong coordinates. Instead of targeting a virus, they lock onto your own healthy cells.
In many cases of autoimmune-related dysautonomia, these autoantibodies go after the nerve receptors that are critical for your autonomic nervous system to work. They essentially jam the signal, blocking or damaging the communication ports on nerve cells so they can't send or receive messages correctly.
It’s like someone putting duct tape over the sensors in a smart home. The main computer can't get accurate readings from the thermostat or security cameras, so the whole system starts going haywire. That’s exactly what happens to your body, leading to the disorienting neurological symptoms of dysautonomia.
The Impact of Chronic Inflammation
Beyond the direct assault from autoantibodies, autoimmune conditions create a state of chronic, low-level inflammation. Picture trying to listen to your favorite song with a constant, nagging static in the background. That’s what systemic inflammation does to your nervous system.
This "inflammatory static" creates a hostile environment for your delicate autonomic nerves. It can:
- Irritate Nerve Fibers: The constant inflammation can make nerves jumpy and over-reactive, leading to unstable function.
- Damage Nerve Structures: Over time, this environment can physically damage the nerves or their protective coating (the myelin sheath).
- Disrupt Blood Flow: Inflammation can also mess with the tiny blood vessels that feed your nerves the oxygen and nutrients they need to work properly.
This is why getting the underlying autoimmune condition under control is so important. When you can dial down the inflammation, you quiet that static and give your nervous system a fighting chance to function better. This is especially true when we look at the connection between conditions like POTS and the vagus nerve, since inflammation can directly sabotage this nerve’s ability to keep things running smoothly.
The connection is clear: when the immune system is in a constant state of high alert, the nervous system pays the price. The resulting symptoms—from brain fog and digestive distress to wild heart rate swings—are the direct fallout from this internal conflict.
Common Autoimmune Culprits
While a lot of autoimmune diseases can have dysautonomia as a sidekick, some are more notorious for it than others. These conditions are often defined by autoantibodies or inflammatory processes that have a known history of targeting neurological tissue.
The infographic below shows just how tangled the web between dysautonomia and other common conditions can be.
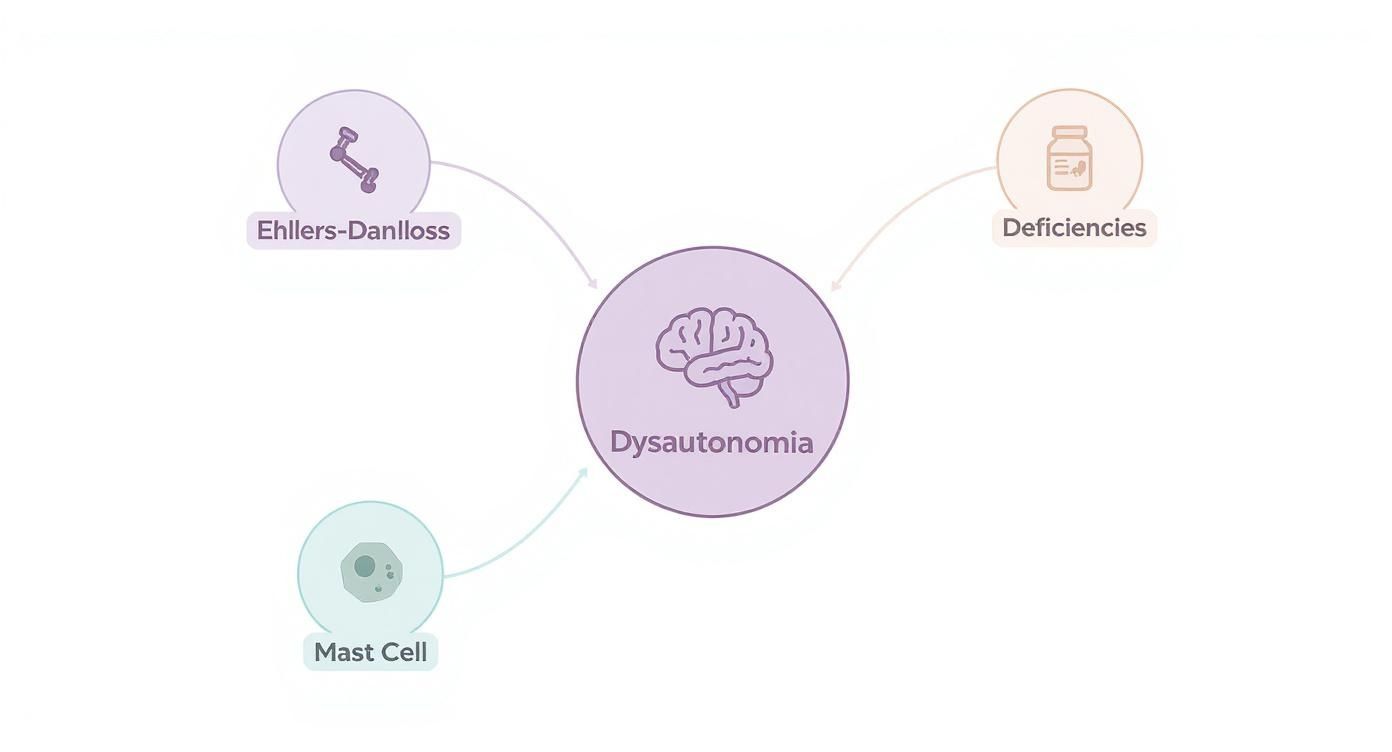
This visual makes it clear that these aren't isolated issues but are often deeply interconnected, creating a complex puzzle of symptoms for patients and doctors to solve.
To help you connect the dots, we've put together a table of common autoimmune conditions and the dysautonomia symptoms they frequently trigger.
Common Autoimmune Diseases Linked to Dysautonomia
| Autoimmune Disease | Commonly Associated Dysautonomia Symptoms | Primary Mechanism (e.g., Inflammation, Autoantibodies) |
|---|---|---|
| Sjögren's Syndrome | POTS, orthostatic hypotension, gastroparesis, severe fatigue, small fiber neuropathy | Autoantibodies targeting nerve receptors, Inflammation |
| Lupus (SLE) | Tachycardia, blood pressure instability, GI dysmotility, Raynaud's phenomenon | Widespread systemic inflammation, Autoantibodies |
| Hashimoto's Thyroiditis | Heart palpitations, temperature intolerance, fatigue, brain fog | Systemic inflammation, Hormonal imbalance |
| Rheumatoid Arthritis (RA) | Orthostatic hypotension, abnormal sweating, cardiovascular autonomic neuropathy | Systemic inflammation damaging nerves |
| Celiac Disease | POTS, syncope (fainting), gastroparesis, peripheral neuropathy | Inflammation, Autoantibodies, Nutrient malabsorption |
| Multiple Sclerosis (MS) | Bladder dysfunction, bowel issues, orthostatic hypotension, heat intolerance | Autoantibodies attacking myelin sheath, Inflammation |
This table isn't exhaustive, but it highlights some of the most well-documented connections. Recognizing that an autoimmune process could be the engine driving neurological symptoms is a huge step forward. It shifts the focus from just chasing individual dysautonomia symptoms to calming the root cause—creating a path toward more effective care that supports both the immune and nervous systems.
Navigating Your Path to an Accurate Diagnosis
Getting the right diagnosis when you’re dealing with the complex overlap of dysautonomia and autoimmune disease can feel like an impossible uphill climb. So many families tell us the journey is long and frustrating, leaving them feeling exhausted and unheard. But you can shift from being a passive patient to an empowered advocate for your health with a structured, proactive approach.
It all starts with becoming the world's leading expert on your own body. Vague complaints are, unfortunately, easy for busy doctors to dismiss. Detailed, organized data is much harder to ignore. Systematically tracking symptoms provides the clear, objective evidence your healthcare team needs to connect the dots and see the full picture.
Become a Detective of Your Own Health
Your most powerful tool, right from the start, is a symptom journal. Don't just jot down "felt dizzy today." The real magic is in the details. Capturing the specifics helps reveal the patterns that are absolutely crucial for a diagnosis.
For every symptom, try to capture these key details:
- What it feels like: Is the dizziness a spinning sensation, or is it more like you’re about to faint? Is your fatigue a heavy, can’t-get-out-of-bed feeling, or is it that "wired but tired" sensation?
- When it happens: Note the time of day and what you were doing. Were you sitting, standing, or lying down when it started?
- How long it lasts: Was it over in a few seconds, or did it linger for minutes or hours? Does it come and go in waves?
- Potential triggers: Did you just eat a specific food? Experience a stressful event? Stand up too quickly?
- Severity: A simple 1-10 scale can be incredibly helpful. Rating the intensity helps you and your doctor track whether things are trending better or worse over time.
This detailed log isn't just for your own reference; it's a critical piece of evidence to bring to your appointments. You’re essentially turning your personal experience into a data set, giving your doctors tangible information to work with.
Understanding Key Diagnostic Tools
Once you present your detailed symptom log, your doctor might suggest specific tests to get to the bottom of things. The list of potential tests can feel intimidating, but understanding what they do can help demystify the process and ease some of the anxiety.
The Tilt Table Test is often considered the gold standard for diagnosing conditions like POTS. During this test, you're safely secured to a table that is slowly tilted upright. The medical team watches your heart rate and blood pressure very closely to see how your body responds to the simple change in gravity. It's a safe, controlled way to reproduce your symptoms so they can be measured objectively.
The point of these tests isn’t to make you feel bad. It's to capture the physiological data that proves your autonomic nervous system isn't working as it should. This is the concrete proof that validates everything you've been feeling.
Other common tests you might encounter include:
- QSART (Quantitative Sudomotor Axon Reflex Test): A fancy name for a test that measures the function of the nerves controlling your sweat glands.
- Autonomic Breathing Test: This looks at how your heart rate and blood pressure react to different, controlled breathing patterns.
- Skin Biopsy: In some cases, a tiny skin sample is taken to check for damage to small nerve fibers, which is a common finding in certain types of dysautonomia.
Assembling Your Expert Healthcare Team
Figuring out the connection between dysautonomia and autoimmune disease is rarely a one-doctor job. More often than not, it takes a collaborative team of specialists, each bringing their unique expertise to your care. Building this team is a critical step on your path to getting real answers.
Your team might include:
- A Rheumatologist: They are essential for diagnosing and managing the underlying autoimmune component.
- A Neurologist or Cardiologist: The key is to find one with a special interest in autonomic disorders. They’re the ones who will order and interpret tests like the Tilt Table Test.
- An Electrophysiologist: This is a cardiologist who specializes in the heart's electrical system and can be incredibly helpful in managing POTS and related conditions.
Never be afraid to seek a second opinion or to find doctors who are known for working with complex, chronic illnesses. A provider who truly listens, believes you, and is willing to work as part of a team is your most valuable asset on this journey.
Building Your Integrated Management Toolkit

Moving from a diagnosis to managing daily life is a huge mental shift. It's about moving away from just reacting to symptoms and instead building a proactive toolkit of strategies that support both your nervous system and your immune system. This integrated approach helps you intentionally manage the tricky intersection of dysautonomia and autoimmune disease, putting you back in the driver's seat of your own health.
Think of your management plan like a well-stocked toolbox. You won't need every single tool every day, but just knowing you have the right options ready for different situations is incredibly empowering. This toolkit is all about combining targeted medical treatments with powerful, foundational lifestyle adjustments.
Laying the Medical Foundation
The first layer of your plan is working closely with your healthcare team to get to the bottom of what's driving your symptoms. This isn't about looking for a single "magic bullet," but about creating a stable base you can build upon.
Medical interventions usually have two main goals: calming down the autoimmune response and getting your autonomic function back on track.
- Immune System Modulation: For the autoimmune side of things, doctors might prescribe immunosuppressants or immunomodulatory drugs. These medications essentially turn down the volume on the "friendly fire," reducing the inflammation and autoantibody attacks that are damaging your nervous system.
- Autonomic Symptom Management: To tackle the dysautonomia symptoms head-on, you might be prescribed beta-blockers for a racing heart, fludrocortisone to help your body hold onto salt and water for better blood volume, or midodrine to tighten blood vessels and stop blood pressure from dropping.
This two-pronged medical approach is crucial. It simultaneously addresses the root cause (the autoimmune attack) and provides relief from the most disruptive daily symptoms (the autonomic dysfunction), creating stability and improving your quality of life.
Fueling Your Body for Stability
What you eat can either add fuel to the inflammatory fire or help to put it out. Adopting a strategic, nutrient-dense diet is one of the most powerful tools you have. The goal is to lower inflammation while helping to stabilize your autonomic nervous system.
An anti-inflammatory diet is a fantastic strategy for managing an overactive immune system. This usually means focusing on whole, unprocessed foods packed with antioxidants and healthy fats. You can dive deeper into specific dietary approaches in our guide on how to reduce inflammation.
At the same time, specific adjustments for dysautonomia are essential. For many people with POTS, increasing salt intake (up to 10 grams per day with your doctor's okay) and fluids (2-3 liters per day) is a total game-changer. This simple strategy helps boost blood volume, making it much easier for your body to keep your blood pressure stable when you stand up.
Incorporating Gentle Movement and Stress Reduction
When you're feeling exhausted and dizzy, the idea of exercise can feel completely overwhelming. But gentle, consistent movement is incredibly important for "retraining" your autonomic nervous system. The goal here isn't intense cardio; it's all about progressive, mindful activity.
Consider these gentle exercise protocols:
- Recumbent Exercises: Think recumbent bikes, rowing machines, or swimming. These activities let you build cardiovascular strength without having to be upright, which helps prevent blood from pooling in your legs and triggering symptoms.
- Strength Training: Focus on floor-based exercises like glute bridges and leg lifts, or use resistance bands while sitting down. Building muscle in your lower body acts like a set of natural compression socks, helping to push blood back up toward your heart and brain.
- Mindful Movement: Practices like yoga and tai chi are brilliant for improving balance, body awareness, and the mind-body connection—all vital for regulating your nervous system.
Finally, managing stress is non-negotiable. The stress hormone cortisol directly fuels inflammation and can send an already sensitive nervous system into overdrive. Techniques like deep diaphragmatic breathing, meditation, and mindfulness actively switch on your parasympathetic nervous system—your body's "rest and digest" mode. Even just five minutes of focused breathing can help shift your nervous system out of high alert, creating a calmer internal environment where your body can heal and regulate itself more effectively.
A Neuro-Tonal Approach to Nervous System Regulation
Once medical treatments and lifestyle changes are in place, many families start looking for other supportive therapies to round out their care plan. This is often where neuro-tonal chiropractic care comes in—it’s an approach focused on gently reducing stress on the nervous system so it can better regulate and adapt on its own.
Picture your nervous system as a highly advanced computer that’s completely overloaded, frozen on high alert. This approach doesn't try to fix the software bug—that’s the job of medical treatments for the autoimmune condition itself. Instead, it acts like a gentle "soft reboot" for the hardware.
The whole goal is to calm the entire system down, helping it shift out of that constant "fight-or-flight" state and back into a more balanced, "rest-and-digest" mode. When that happens, the body has a much better internal environment to work with.
Easing Stress on the Master Control System
A neuro-tonal approach uses very precise and gentle adjustments to address areas where tension and stress have gotten stuck in the nervous system. This is a huge deal when you're dealing with the overlap of dysautonomia and autoimmune disease, since the system is already under so much strain from inflammation and scrambled communication signals.
This isn’t about forceful cracking or popping. It’s all about improving the tone—or the resting state—of the nervous system. An unbalanced tone is a lot like a guitar string that’s been wound way too tight; it makes a harsh, jarring sound and is always on the verge of snapping. By gently loosening that tension, you can restore harmony and resilience to the system.
A well-regulated nervous system simply has a greater capacity to handle stressors. This means that while the underlying conditions are still there, the body can become better equipped to manage symptoms and adapt to daily challenges without getting so easily overwhelmed.
A Supportive Piece of the Wellness Puzzle
It's really important to understand that this isn’t a cure. Neuro-tonal care is a supportive strategy, one designed to help your body function at its absolute best while you navigate a chronic illness. By improving the fundamental communication pathways between the brain and the body, this approach can help:
- Enhance Resilience: A calmer nervous system is a more resilient one, better able to handle the physical and emotional bumps in the road.
- Support Self-Regulation: It aims to improve the body’s own built-in ability to manage functions like heart rate, digestion, and sleep patterns.
- Complement Other Therapies: It works right alongside your medical treatments and lifestyle shifts, helping to create a more complete and cohesive care plan.
This approach is especially powerful for kids, since early support can help a developing nervous system build a strong foundation for a lifetime of wellness. Helping to clear interference and improve regulation from a young age can make a world of difference. To get a deeper look at the nervous system's incredible capacity for healing, you can read our guide on how to repair your autonomic nervous system.
Integrating this gentle care can be one more powerful piece in your family's comprehensive wellness puzzle.
Frequently Asked Questions
When you're trying to connect the dots between dysautonomia and autoimmune disease, it’s completely normal to have a lot of questions. We’ve put together some straightforward answers to the things we hear most often, giving you clarity and confidence as you navigate your family's health.
Can Treating My Autoimmune Disease Improve My Dysautonomia Symptoms?
Yes, for many people, it absolutely can. Think of it this way: the autoimmune condition is like a storm of inflammation and misdirected antibodies raging inside the body. That storm can easily knock out the power grid—your autonomic nervous system.
When you start treatments that calm that autoimmune storm, you’re essentially getting the power back on. This is why so many people see a real drop in their autonomic symptoms, like less fatigue, clearer thinking, and a more stable heart rate, once their autoimmune condition is better managed.
By getting to the root of the autoimmune trigger, you're quieting the chaos that's scrambling your nervous system's signals. It's often a game-changer for overall function and quality of life, really showing how deeply these two conditions are linked.
What Kind of Doctor Should I See if I Suspect Both Conditions?
Building the right healthcare team is crucial, and it's definitely a team sport. Your first stop is usually your primary care physician, but from there, you’ll likely need a couple of key specialists on your roster.
A rheumatologist is the expert in diagnosing and managing autoimmune diseases. For the dysautonomia side of things, you'll want a neurologist or a cardiologist who specializes in autonomic disorders. The most important part? Making sure these doctors talk to each other. When your specialists work together, you get a cohesive plan that treats the whole picture, not just separate pieces.
Are There Lifestyle Changes That Help Both Conditions?
Absolutely! This is where you can take back a lot of control. Making smart lifestyle choices can provide a powerful foundation for calming both your immune system and your nervous system.
- Eat to Calm Inflammation: An anti-inflammatory diet does double duty, helping to soothe the autoimmune response while also giving your nervous system the nutrients it needs to function well.
- Move Gently, but Consistently: You don't need intense workouts. Gentle, steady movement like swimming, walking, or using a recumbent bike can significantly improve autonomic function without causing a flare-up.
- Master Your Stress: Your nervous and immune systems are highly sensitive to stress. Simple practices like mindfulness, deep breathing exercises, or even just quiet time can make a world of difference in regulating both.
These aren't just temporary fixes for symptoms; they’re about creating a healthier, more stable internal environment where your body can begin to heal and find balance.
At First Steps Chiropractic, we see this intricate connection between the nervous and immune systems every day. Our gentle, neuro-tonal approach is specifically designed to take the stress off the body's master control system, helping it better regulate and adapt on its own. To see how our pediatric and family-focused care can support your wellness journey, visit us at https://firststepschiropractic.com.

