When you first hear the words "low muscle tone" or "hypotonia," it’s easy to feel a wave of concern, especially when they're tied to developmental delays. It’s a completely normal reaction. The connection makes sense once you break it down: low muscle tone simply means a child's muscles are more relaxed at rest, so it takes more effort for them to move and hold themselves steady. This extra work can naturally slow down the process of hitting those big milestones, creating a clear link between low muscle tone and developmental delay.
What Low Muscle Tone Means for Your Child's Development

Let's clear up a common misunderstanding right away. Many parents hear "low tone" and think it means their child's muscles are weak, but that’s not the full picture. It’s really about the muscle's readiness to work.
Here’s a helpful way to think about it: imagine muscle tone is like the tension in a rubber band. A typical rubber band is already taut, ready to snap into action the moment you need it. But a rubber band with low tone is loose and floppy. To get that same snap, you first have to pull out all the slack.
That's exactly what's happening for a child with hypotonia. Their muscles are like that loose rubber band, so their brain has to send stronger signals and they have to use more energy just to get going. This isn't an issue of muscle strength itself, but rather the communication coming from the nervous system.
From Floppy to Functional
The central nervous system—the brain and spinal cord—is the command center telling the muscles how much tension they should hold at all times. If those signals aren't firing just right, the muscles stay in a more relaxed state. This makes it a real challenge for a child to do things we take for granted, like holding up their head, sitting upright, or initiating movement.
The most important thing to remember is that hypotonia is usually a symptom, not the root cause. It's a sign that the brain-body connection needs a little extra support to work more smoothly.
This guide is designed to help you move past the worry and step into a place of empowerment. We're going to walk through the "what" and "why" of low muscle tone, giving you a clear roadmap for the path ahead. Together, we'll explore:
- The underlying causes and different types of hypotonia
- How low tone can create a domino effect on developmental milestones
- The signs to look for and what the diagnostic process involves
- Effective, evidence-based therapies that build both strength and coordination
- A clear action plan to support your child’s progress every step of the way
By understanding the real connection between low muscle tone and developmental delay, you can become your child's best advocate. With the right support and interventions, you can help them build the strong foundation they need to thrive.
Understanding the Roots of Hypotonia
To really get to the bottom of low muscle tone and developmental delay, we have to look deeper than the muscles themselves—we need to see what’s going on inside your child’s nervous system. Muscle tone isn't about strength or how big a child's muscles are. It's about the subtle, constant tension a muscle holds even when it's resting, keeping it ready for action. This state of readiness is managed by a non-stop conversation between the brain and the muscles.
Think of it like a car idling at a stoplight. The engine isn't actively propelling the car forward, but it's on, humming, and ready to go the instant the light turns green. For a child with hypotonia, that idle is set way too low. The engine is on, but it’s sputtering and needs a lot more gas (or energy) just to get the car moving.
This is a key reason why it's so important to know the difference between low tone and true muscle weakness. Hypotonia is a neurological issue tied to that low "idle speed." Muscle weakness, on the other hand, is when the muscle itself can't produce enough force. A child can actually have normal strength but still struggle with low tone because the initial signal to get moving is weak or inefficient.
Central vs. Peripheral Hypotonia
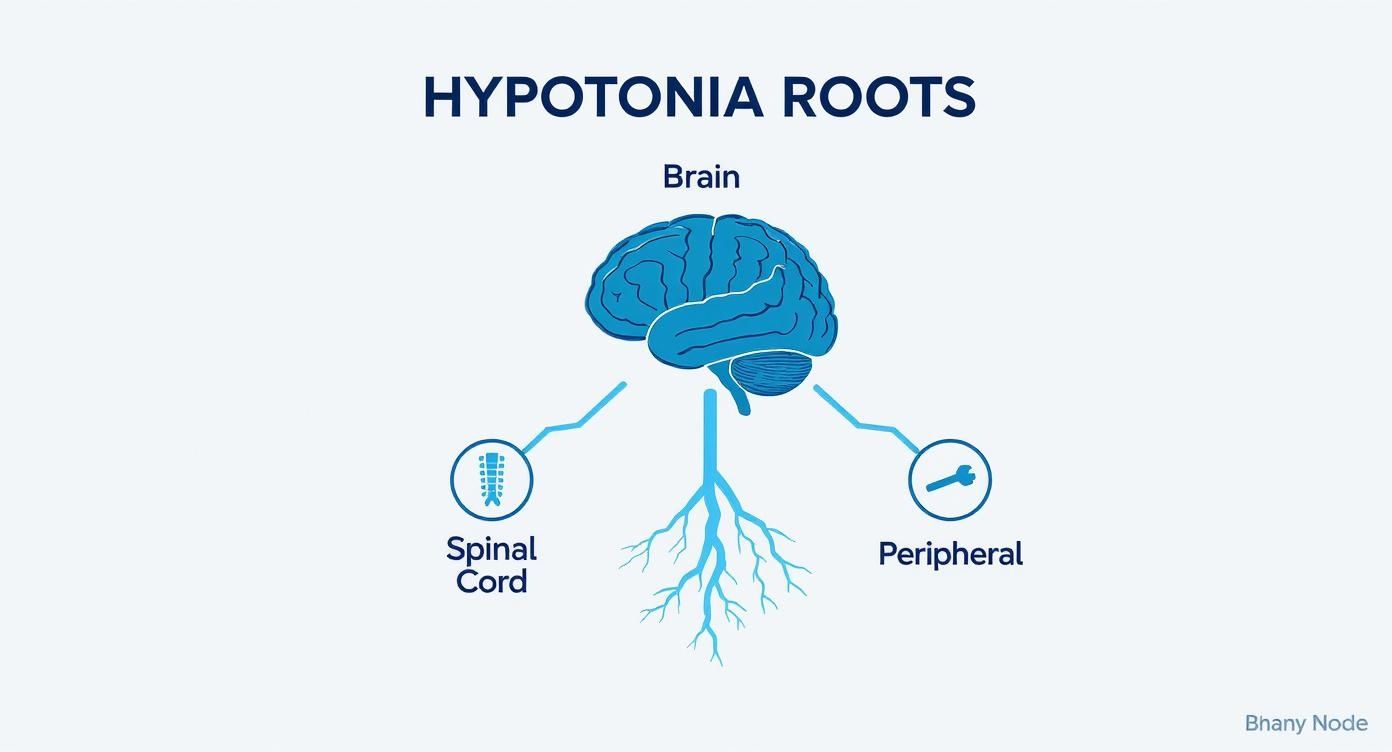
Because hypotonia is a symptom, not a diagnosis, figuring out its origin is crucial. Healthcare providers usually break it down into two main types, depending on where the communication breakdown is happening:
-
Central Hypotonia: This is the most common kind, and it starts in the central nervous system—the brain or the spinal cord. Anything that affects the brain before, during, or after birth can mess with the signals that are supposed to regulate muscle tone.
-
Peripheral Hypotonia: This type is rooted in the peripheral nervous system. The problem might be with the nerves that travel from the spinal cord to the muscles, at the junction where the nerves and muscles connect, or within the muscles themselves.
Recognizing that hypotonia is a symptom is the first real step toward getting answers. It’s like a big, clear signpost pointing toward an underlying cause that needs our attention. For so many parents, understanding the "why" behind their child's struggles is a huge part of the journey. To dig into this a bit more, you can check out our guide on what causes developmental delays.
A Reliable Early Red Flag
The presence of hypotonia is often one of the first and most reliable signs that a child may face developmental challenges. Its impact isn't just on motor skills; it can send ripples across a child’s entire developmental landscape.
Hypotonia, defined as decreased muscle tone or generalized floppiness, functions as a reliable early "red flag" for developmental disorders. It is found consistently across several neuromuscular, metabolic, and genetic disorders and frequently coexists with global developmental delay.
This condition doesn't just delay motor milestones like sitting up or walking. It can also lead to secondary issues like torticollis (an abnormal, tilted neck posture) because of the ongoing muscle imbalances. That’s why addressing hypotonia is about so much more than movement—it’s about supporting the entire foundation of a child’s body. Pinpointing the source of the low tone is the cornerstone of building a targeted, effective support plan to help your child thrive.
How Hypotonia Creates a Domino Effect on Milestones
Low muscle tone isn't just a simple issue affecting a child's arms or legs. It’s a foundational problem that can set off a chain reaction across every single area of development.
Picture a child's developing body like a building under construction. Before you can even think about putting up walls, running electrical, or installing windows, you absolutely must have a strong, stable foundation. In a child's development, that foundation is core strength.
When a child has low muscle tone, the muscles of their trunk and around their spine—their core—are usually the most impacted. These muscles are meant to be a steady base, a central anchor from which all other movements can begin. Without that stability, the whole structure becomes wobbly and inefficient.
The First Domino to Fall: Gross Motor Skills
The very first milestones a baby works towards are all about fighting gravity, and that requires a ton of core engagement. It’s no surprise, then, that these fundamental gross motor skills are the first to take a hit when hypotonia is present.
- Lifting the Head: During tummy time, a baby with low tone has to work so much harder just to lift their heavy head off the mat. This often leads to frustration, and pretty soon, they start avoiding tummy time altogether.
- Rolling Over: This isn't a simple movement; it requires a coordinated sequence of effort from the neck, back, and abdominal muscles. When the core is "floppy," it's incredibly difficult to get that sequence started, let alone completed.
- Sitting Independently: Without enough trunk stability to hold themselves upright, a baby will often slump forward or lean to one side. They just can't maintain that posture without support, long after their peers have mastered it.
Because these early skills are the building blocks for more advanced movements like crawling and walking, a pattern of low muscle tone and developmental delay quickly starts to take shape. Each milestone that's missed or delayed makes the next one that much harder to reach.
The Chain Reaction: Fine Motor, Feeding, and Speech
But the domino effect doesn't stop with the big movements. It’s surprising how much a stable core matters for all the small, precise actions, too. When a child is constantly using all their energy just to keep their body from slumping over, there’s very little stability or focus left for their hands and mouth to do their jobs.
This concept map shows how hypotonia, which starts in the nervous system, can spread its effects to so many different areas.
Whether the origin of the issue is central (brain and spinal cord) or peripheral (the nerves extending out), the result is the same: a major disruption to the body's foundational stability.
This instability has a direct impact on the finer skills:
- Fine Motor Skills: Imagine trying to write your name while sitting on a wobbly stool. That’s a bit like what a child with a weak core feels all the time. It makes it incredibly tough to control the small muscles in their hands for things like grasping a toy, using a pincer grasp to pick up a cheerio, or bringing their hands to their mouth to explore.
- Feeding and Swallowing: Hypotonia often affects the muscles in the jaw, tongue, and cheeks. This can lead to a weak suck when nursing or drinking from a bottle, difficulty chewing solid foods, and trouble managing food in the mouth. Sometimes, this can result in feeding aversions or challenges with weight gain.
- Speech and Language: The same oral muscles that are used for eating are also critical for making speech sounds. Low tone can make it difficult for a child to form sounds clearly, which often leads to unclear articulation and delayed language. You can learn more about this connection in our detailed guide on what is speech delay.
This table breaks down how a single root cause—low muscle tone—can branch out to create challenges across so many different parts of a child's development.
Impact of Low Muscle Tone Across Developmental Domains
| Developmental Domain | How Low Muscle Tone Affects It | Common Examples of Delays |
|---|---|---|
| Gross Motor | Lack of core stability makes it hard to fight gravity and coordinate large muscle groups. | Difficulty with head control, rolling, sitting up, crawling, walking. |
| Fine Motor | Without a stable trunk, the small muscles in the hands lack a secure base for precise movements. | Trouble with grasping objects, pincer grasp, bringing hands to midline, self-feeding. |
| Oral Motor/Feeding | Weakness in the jaw, cheek, and tongue muscles impacts sucking, chewing, and swallowing. | Poor latch, difficulty with bottle/cup, trouble managing different food textures. |
| Speech & Language | The same oral motor weakness makes it difficult to articulate sounds clearly. | Unclear speech, delayed babbling, difficulty forming words, drooling. |
| Sensory/Social | Constant effort to maintain posture can be draining, leading to fatigue and reduced engagement. | Overwhelmed easily, avoids physical play, delayed social interaction. |
As you can see, the challenges are all interconnected, stemming from that initial lack of muscle stability.
This progression from gross motor to fine motor and oral motor challenges is a classic example of the developmental domino effect. When the foundational piece—core stability—is unsteady, it creates a ripple effect that touches nearly every aspect of a child's early life.
Research backs this up, showing that early motor delays can be a strong predictor of later challenges. For example, studies on children with ASD, where hypotonia is quite common, have found a powerful link between delayed walking and later language deficits. One study noted that among autistic children, 71.5% had motor milestone delays, and hypotonia was a factor for about 32.3% of them. That same study showed that delayed walking was strongly correlated with an absence of verbal language by age 4.
Understanding this chain reaction is so important. It shows us that by getting to the root issue of low muscle tone with the right therapies and support, we can help get all those developmental dominoes lined up again, ready to fall in the right order and at the right time.
Navigating the Diagnostic Journey for Low Muscle Tone
As a parent, your intuition is your superpower. You know your child better than anyone, and you’re often the first person to sense when something might be a little off. Recognizing the early signs of low muscle tone is the first real step on the path to getting answers, turning that nagging feeling of concern into confident, proactive steps.
The journey to a diagnosis rarely starts with a complex test. It begins with those small, everyday observations you make. Maybe you've noticed your newborn feels especially "floppy" or "like a rag doll" when you lift them from the crib. Or perhaps they struggle to get a good latch during feeding time. These little clues are actually crucial pieces of the puzzle.
Trusting what you see and sharing those concerns with your pediatrician is the most important next move you can make. This isn't about looking for something to be wrong; it's about being your child's best advocate so they have every opportunity to thrive.
What to Expect at the Pediatrician's Office
When you bring up concerns about low muscle tone and developmental delay, your pediatrician will likely start with a few key in-office checks. These are gentle, hands-on evaluations designed to see how your child’s muscles and reflexes are responding. They aren't trying to land on a diagnosis right then and there, but rather gathering the first round of information to see the bigger picture.
A very common assessment you'll see is the pull-to-sit maneuver. Here, the doctor will gently pull your baby up from a lying position to a sitting one, watching to see how much their head lags behind their body. A noticeable head lag can be an early sign of low tone in the neck and core muscles.
Other things they’ll look for might include:
- Observing Posture: How does your baby hold their body when they're just resting? Do they tend to slump, or do they have that "frog-leg" posture where their hips splay out to the sides?
- The Scarf Sign: The doctor gently takes one of your baby's arms and draws it across their chest, like a scarf. For a baby with hypotonia, the elbow might cross the midline of the body with very little resistance.
- Vertical Suspension: When the doctor holds your child up under their arms, a child with low tone might feel like they could slip right through their hands because of instability in the shoulder area.
Your doctor will also ask a lot of questions about your child's developmental milestones, feeding patterns, and general behavior. Coming prepared with specific examples can make this conversation incredibly helpful.
Think of this initial visit as a fact-finding mission. Your pediatrician is your primary partner, helping you connect your own observations with clinical findings to map out the best next steps.
Before we dive into specialist referrals, it's helpful for parents to know what to look for at home. Early recognition is key, and certain signs are more common at specific stages.
Age-Based Red Flags for Low Muscle Tone
This checklist can help you pinpoint specific observations based on your child's age. If you notice a consistent pattern of these signs, it’s a good reason to start a conversation with your pediatrician.
| Age Range | Potential Signs and Symptoms |
|---|---|
| 0-3 Months | – Feels "floppy" or like a rag doll when held. – Difficulty lifting their head during tummy time. – Weak cry or trouble sucking and swallowing. |
| 3-6 Months | – Significant head lag when pulled to a sitting position. – Does not push up on arms during tummy time. – Trouble bearing weight on legs when held in a standing position. – Seems to "slump" when placed in a supported sitting position. |
| 6-12 Months | – Delayed rolling over, sitting up without support, or crawling. – Uses unusual crawling patterns (e.g., pulling self with arms only). – Does not pull up to a stand. – Prefers to "W-sit" (sitting with knees bent and legs fanned out). |
| 12+ Months | – Delayed walking (typically after 18 months). – Clumsy or uncoordinated movements; frequent falling. – Tires very easily during physical play. – May have difficulty chewing and swallowing solid foods. |
Remember, every child develops at their own pace. This table isn't for diagnosing, but for empowering you with information so you can have a more productive discussion with your child’s healthcare team.
When a Specialist Referral Is Needed
Sometimes, that first evaluation gives your pediatrician enough information to recommend therapies like Early Intervention right away. But if the hypotonia seems more significant or if there are other red flags, they will likely refer you to a specialist for a deeper look.
Getting a referral is a positive step. It means you’re moving closer to understanding the root cause of the low muscle tone. The two most common specialists you’ll be connected with are:
- Pediatric Neurologist: This doctor is an expert on the brain, spinal cord, and nervous system. They’ll conduct a more detailed neurological exam and might order tests like a brain MRI or an EMG to check how the nerves and muscles are communicating.
- Developmental Pediatrician: This specialist looks at the whole child—motor skills, cognitive function, speech, and social development. They are masters at identifying specific delays and building a comprehensive support plan that addresses all areas of need.
This part of the process can feel overwhelming, but each specialist brings another layer of expertise to your child’s care team. Their job is to rule out or identify any underlying conditions and make sure the therapy plan is perfectly tailored to your child’s unique needs. This is how we demystify the connection between low muscle tone and developmental delay, giving you the clarity and knowledge to advocate for your child with confidence.
Effective Therapies That Build Strength and Skill

Knowing the link between low muscle tone and developmental delay is the first step. The next is to find the right support to help your child thrive. Once you have a clearer picture of your child’s needs, you can start building a team of dedicated professionals who will work together to build strength, improve coordination, and help your child master essential life skills.
Think of it as creating a support structure around your child, where each therapy is a crucial pillar. Physical Therapy lays the foundation of strength, Occupational Therapy adds the functional details for daily living, and Speech Therapy ensures clear communication. Together, they create a complete plan that addresses your child's unique challenges from every angle.
Physical Therapy: The Foundation of Strength
For most kids with hypotonia, Physical Therapy (PT) is the first and most important intervention. A pediatric physical therapist's main goal is to improve core stability, balance, and the gross motor skills that involve large movements of the arms, legs, and torso.
They are essentially the architects of your child's foundational strength. Through targeted, play-based exercises, a PT helps your child’s nervous system and muscles finally learn to work together as a team.
Key areas a physical therapist will focus on include:
- Building Core Strength: This is the absolute cornerstone. A stable core is non-negotiable for everything from sitting up straight to running and jumping.
- Improving Balance and Coordination: Therapists use fun activities, like walking on squishy surfaces or balancing on one foot, to help your child feel more secure and confident in their movements.
- Achieving Motor Milestones: PTs design engaging routines to help children master skills like rolling over, crawling, pulling up to stand, and eventually, walking.
A pediatric physical therapist does more than just lead exercises; they teach your child’s body how to activate and coordinate muscles in the right sequence, turning wobbly effort into effective movement.
Occupational Therapy: Skills for Daily Living
While PT focuses on the big picture of movement, Occupational Therapy (OT) zooms in on the practical, everyday tasks that allow a child to be independent. An OT helps your child participate fully in their most important "occupations"—which for a child, means playing, learning, and taking care of themselves.
When low muscle tone and developmental delay get in the way of fine motor skills, an OT is the specialist who can bridge that gap. They work on the precise hand and finger movements needed for things like holding a crayon, using a fork, or buttoning a shirt.
OTs also address other critical areas:
- Sensory Integration: Many children with hypotonia also struggle with sensory processing. OTs design activities to help the brain better understand and respond to the world around them.
- Activities of Daily Living (ADLs): This includes everything from self-feeding and getting dressed to being ready to learn handwriting.
- Visual-Motor Skills: These skills are essential for hand-eye coordination, like catching a ball or putting puzzle pieces together.
Speech Therapy: The Power of Communication
The effects of low muscle tone don’t stop at the limbs; they often extend to the small, intricate muscles in the face, jaw, and tongue. This is where a Speech-Language Pathologist (SLP) becomes a vital part of the team.
An SLP's work goes far beyond just making sounds correctly. They focus on strengthening the underlying muscle control needed for a child to eat safely and speak clearly.
Their interventions often target:
- Oral Motor Strength: Exercises to strengthen the lips, tongue, and jaw help improve chewing, swallowing, and even managing drool.
- Articulation: SLPs use specific techniques to teach a child how to produce speech sounds that are difficult because of low muscle tone.
- Feeding Therapy: For kids who have a weak suck or struggle with different food textures, an SLP provides strategies to make mealtimes safer and more enjoyable.
Early Intervention: A Critical First Step
For children under the age of three, Early Intervention (EI) is a game-changer. It's a publicly funded program that provides access to these vital therapies right in your home or another natural setting. EI is a critical first line of support, often available at no cost to families.
These services are designed to address developmental delays as early as possible, because we know the first few years of life are a crucial window for brain development. If you have any concerns at all, you can request an EI evaluation without even needing a doctor’s referral.
Assembling a well-rounded care team is the most powerful thing you can do. While these therapies are the core of most plans, many parents also explore complementary approaches, like neurologically-focused pediatric chiropractic, to support the nervous system's role in all this. As your child builds foundational stability, you may also want to learn how to strengthen core muscles through fun activities you can do at home.
Your Action Plan for Supporting Your Child
Knowing something is one thing, but turning that knowledge into action is where the real power lies. When you're navigating the world of low muscle tone and developmental delays, it can feel overwhelming. But having a clear, proactive plan makes all the difference. This roadmap is designed to help you step confidently into your role as the most important member of your child’s care team.
The first steps happen right at home, well before you ever see a specialist. Start by becoming a keen observer. Keep a simple log of what you see—not just the big milestones your child might be missing, but the small, everyday details. How do they move? What’s their posture like when they sit? Do they get tired more quickly than other kids during playtime? These notes will be incredibly valuable when you talk to your pediatrician.
Preparing for Your Pediatrician Visit
With your observations in hand, you can walk into that pediatrician’s office feeling prepared and confident. This isn't the time to be shy; be direct and ask for exactly what you think your child needs. The goal here is to build a partnership with your doctor to get the right supports in place as quickly as possible.
Here are a few key things to do during that conversation:
- Share Your Written Log: Show your doctor the notes you’ve been taking. This gives them concrete examples to work with instead of just a general feeling of, "I'm concerned."
- Request a Full Developmental Screening: Ask for a formal assessment that can objectively measure where your child is at compared to their peers.
- Advocate for Referrals: Don’t wait to be offered. Directly ask for referrals to specialists who can help, like a pediatric neurologist or a developmental pediatrician, and for therapy services.
You are your child’s number one advocate. A specific request like, “I am concerned about my child’s low muscle tone and would like a referral for a physical therapy evaluation,” is clear, direct, and far more likely to get the ball rolling.
Creating a Supportive Home Environment
While professional therapies are a huge piece of the puzzle, the progress made at home every single day is just as important. You don’t need a bunch of expensive equipment to create a supportive and engaging environment—just a little creativity and consistency.
Weave playful, strength-building activities into your daily routine. Get creative with tummy time by propping your baby over a rolled-up towel or your leg to make it a little easier and more engaging. For toddlers, simple things like building obstacle courses with pillows or playing "animal walks" (like bear crawls and frog jumps) are fantastic for building core strength.
The need for early and consistent support can’t be overstated. It's estimated that 317 million children and young people worldwide live with health conditions connected to developmental delays. Getting ahead of it with proactive intervention is key, as it can help reduce the long-term health risks that can come with early muscle tone issues. You can learn more about these global health findings directly from the World Health Organization.
By observing, advocating, and creating a playful environment at home, you’re building a powerful foundation for your child. With your support and a dedicated care team, kids with low muscle tone can make incredible progress and truly thrive.
At First Steps Chiropractic, we’re focused on supporting your child’s neurological development right from the start. If you’re looking for a gentle, neurologically-focused approach to add to your child’s care plan, we’d love to show you how we help families here in Hayden, ID. Visit us at https://firststepschiropractic.com to schedule a complimentary consultation.

