If you’ve ever noticed your child seems a bit more "floppy" than their friends or has a tough time with posture, you might be seeing signs of low muscle tone. This is a super common co-occurrence with autism. It’s not about muscle weakness, but about how ready a muscle is to move. Getting a handle on this connection is the first step toward giving your child the right support to thrive.
The Connection Between Autism and Low Muscle Tone

Hearing the term "low muscle tone" can sound a little scary for parents, but it's a very common and manageable part of the autism spectrum.
To really get it, think of a muscle like a rubber band. A muscle with typical tone is like a rubber band that’s already slightly stretched—it’s taut and ready to spring into action at a moment's notice.
A muscle with low tone, also known as hypotonia, is more like a relaxed, limp rubber band. It’s not weak or damaged, it just needs more effort and a bit more time to tighten up and get a job done. That difference in "at-rest" tension is at the very core of the motor skill challenges some kids with autism face.
Why This Link Matters
The link between autism and low muscle tone is a big deal. Research actually shows that about 50% of children with autism spectrum disorder (ASD) also experience hypotonia. That makes it an incredibly common part of the picture.
This affects everything from a child’s ability to sit up straight in a classroom chair to how they hold a pencil. Not surprisingly, this can lead to delays in hitting those big motor milestones. You can get a deeper look into how hypotonia impacts daily life by reviewing the research on this connection.
This guide is here to give you the knowledge you need to navigate this part of your child’s journey. We’re going to cover:
- How to spot the specific signs of hypotonia.
- The real-world impact low muscle tone can have on daily life and learning.
- Effective therapies and simple at-home strategies to help build strength.
Understanding hypotonia isn’t about focusing on a weakness. It's about recognizing how your child’s body works so you can provide targeted support that helps them build confidence and truly thrive in their world.
Grasping this connection provides critical context for why certain tasks might be so much more tiring or difficult for your child. It helps shift the perspective from a potential behavioral issue to a physiological one—which is key for finding support strategies that actually work.
By digging into the nuances of autism low muscle tone, you can become a better advocate for your child’s needs. For more on the neurological side of things, you might be interested in our guide on how chiropractic care supports autism and the nervous system.
How to Spot Signs of Low Muscle Tone in Your Child
Recognizing the signs of low muscle tone in autism, also known as hypotonia, can sometimes feel like trying to solve a puzzle. The clues are often subtle, and it's easy to mistake them for simple clumsiness or even laziness.
But once you know what to look for, you can start piecing together a clearer picture of your child’s motor challenges and become their most powerful advocate. The signs generally fall into two main categories of motor skills.
Challenges with Gross Motor Skills
Gross motor skills are the big movements. They involve the large muscle groups of the body we use for walking, running, and even just sitting upright. For a child with hypotonia, activating these muscles takes a lot more energy, which leads to some very telling behaviors.
You might notice your child has a "floppy" quality, almost like a rag doll. When you pick them up, they might feel heavier than you expect or seem to slip right through your hands.
Other common gross motor signs include:
- A Slumped Posture: They may struggle to sit straight in a chair, often propping themselves up with their hands or slumping over the table.
- W-Sitting: Many kids with low core strength prefer sitting in a "W" position on the floor because it creates a wider, more stable base for them to play.
- Leaning for Support: Does your child constantly lean against walls, furniture, or even you while standing? This is a classic sign they are trying to conserve energy.
- Delayed Milestones: Children with hypotonia often reach milestones like rolling over, sitting up on their own, crawling, and walking later than their peers.
These signs are so important that their presence can be a key indicator that it’s time for a deeper look. In fact, research analyzing data from over 5,000 children with ASD found that hypotonia often acts as an early "red flag." It actually led to an autism diagnosis approximately 1.5 years earlier than in children who didn't have it. You can explore the full study on hypotonia as an early marker for ASD to better understand its diagnostic significance.
Difficulties with Fine Motor Skills
While the bigger gross motor issues are often more obvious, low muscle tone also affects the small, intricate muscles in the hands, fingers, and mouth. These are the muscles we rely on for precise, coordinated movements needed for all sorts of daily tasks.
A child with hypotonia might grip a crayon with their whole fist instead of their fingertips. This isn't a choice—it's a compensation strategy because the smaller, more refined movements are just too exhausting.
Here are some signs your child may be struggling with fine motor skills because of low muscle tone:
- A Weak Grasp: They may have trouble holding onto toys, utensils, or a pencil and often drop items.
- Messy Eating: Difficulty coordinating the muscles in their jaw and tongue can make chewing and swallowing a real challenge.
- Dressing Difficulties: Tasks like buttoning a shirt, zipping a jacket, or tying shoes can be incredibly frustrating for them.
- Tires Easily: They may avoid activities like drawing, building with blocks, or using scissors simply because of the immense effort required.
Observing these specific behaviors—in both big and small movements—gives you incredibly valuable information. It arms you for more productive, detailed conversations with pediatricians and therapists, which is always the crucial first step toward getting your child the right support.
Common Signs of Hypotonia Across Different Age Groups
To help you connect the dots, here’s a quick breakdown of what low muscle tone can look like as a child grows. Keep in mind that every child develops differently, but these are common patterns to watch for.
| Age Group | Gross Motor Signs | Fine Motor Signs | Other Indicators |
|---|---|---|---|
| Infants | Appears "floppy" when held, struggles with head control, delayed rolling or sitting up. | Weak suck when feeding, has trouble bringing hands to mouth, doesn't grasp toys firmly. | Seems overly passive, feels "heavy" when lifted. |
| Toddlers | W-sitting, frequent falls, hesitates with climbing or running, walks with a wide gait. | Fisted grasp on crayons, difficulty using utensils, struggles with stacking blocks. | Tires quickly during play, may have speech articulation issues. |
| School-Aged Children | Slumps at their desk, leans on walls, avoids physical activities like sports, clumsy movements. | Messy handwriting, trouble with buttons and zippers, avoids tasks like cutting with scissors. | Complains of being tired, difficulty with endurance in P.E. class. |
Spotting these signs isn’t about labeling your child, but about understanding their unique needs. When you know what’s really going on, you can find the right path forward to help them build strength, confidence, and skill.
The Neurological Roots of Hypotonia in Autism

To really get to the bottom of autism low muscle tone, we can't just look at the muscles. We have to go straight to the source: the brain, which acts as the body's central command center. Hypotonia isn't just about a child's physical strength; it's deeply connected to the unique way an autistic brain processes and sends signals for movement. This is a neurological difference, not a muscular one.
Think of it like a manager trying to give instructions to a worker over a crackly phone line. If the connection is weak or fuzzy, the message won't get through clearly or quickly. The worker might still get the job done, but it’s going to take a lot more effort and time just to get started.
That’s a great way to picture what’s happening with hypotonia. The real issue is in the communication pathway between the brain and the muscles, which impacts how ready a muscle is to spring into action.
The Cerebellum's Role in Motor Control
One of the key players in all of this is the cerebellum. Tucked away at the back of the head, this part of the brain is the body’s "movement coordinator." It’s in charge of balance, coordination, posture, and getting the timing of our movements just right.
For many autistic individuals, the cerebellum functions a bit differently. It might process signals at another speed or with less precision, and that can directly lead to the reduced muscle readiness we see in hypotonia. This is exactly why tasks that demand smooth, coordinated movements can be so tough.
Motor challenges linked to hypotonia in autistic children often go beyond simple muscle weakness, pointing to the broader neurological systems that manage movement. In fact, studies estimate that over 70% of 8-year-old autistic children show delays in key motor milestones like sitting up, walking on their own, and climbing. You can find more details about the neuromuscular mechanisms in autism on SFARI.org.
Hypotonia in autism is fundamentally a signaling issue. The muscles themselves are typically healthy, but the instructions they receive from the nervous system are less efficient, requiring more conscious effort to produce movement.
The Nerve-Muscle Communication Gap
Another critical piece of the puzzle is the neuromuscular junction. This is the microscopic point where a nerve fiber connects with a muscle fiber to deliver its electrical "go" signal.
For a muscle to contract efficiently, that signal needs to be strong and clear. In cases of hypotonia, the transmission can be less effective. The signal might arrive weaker or travel more slowly, which naturally results in a delayed or reduced muscle response.
This communication gap explains why a child with autism low muscle tone might seem "floppy" or tire out so easily. Their brain has to work so much harder to send a signal that’s strong enough to get their muscles to the right level of tension. Understanding how autism and the nervous system are connected is crucial for finding supportive care. When we recognize these neurological roots, we can find much better ways to support motor development right from the ground up.
How Low Muscle Tone Impacts Daily Life and Learning

Low muscle tone isn't just a clinical diagnosis—it sends ripples through nearly every part of a child's day. For a child with autism low muscle tone, what looks like a simple physical challenge can profoundly affect their ability to learn, play, and become more independent. Understanding this connection is key to figuring out why certain situations are so draining for them.
Imagine you were asked to write an essay while balancing on one foot. You could probably do it, but a huge chunk of your mental energy would be spent just trying to stay upright, leaving very little focus for the actual writing. This is the reality for a child with poor core strength trying to sit through a school day.
Their brain is constantly firing off extra signals just to keep their body stable in a chair. This non-stop effort is mentally and physically exhausting, which directly impacts their ability to pay attention to the teacher and process new information.
From the Classroom to the Playground
The classroom itself can feel like an obstacle course. Weak core and postural muscles make it incredibly difficult for a child to sit still and maintain focus. You might see them constantly shifting their position, slumping over their desk, or propping their head up with their hands—not because they're bored, but out of sheer physical necessity.
This constant physical demand often leads to:
- Reduced Attention Span: When the body is working overtime just to stay stable, the brain has far fewer resources left for learning and concentration.
- Difficulty with Handwriting: A weak grip combined with poor shoulder stability can make writing physically painful, often resulting in messy or illegible work.
- Social Challenges: A child who tires out quickly may start to pull back from physically demanding games on the playground, which can get in the way of forming friendships.
Low muscle tone doesn't just affect how a child moves; it affects how they experience their entire world. The fatigue that comes from simple tasks can impact their mood, their willingness to try new things, and their overall engagement in both social and academic settings.
Building Independence Through Daily Tasks
Beyond school, hypotonia creates real challenges for the self-care routines that are so important for building confidence and independence. So many everyday tasks that we do without a second thought require a surprising amount of fine motor control and strength.
Think about all the small, coordinated movements needed just to get ready for the day. For a child with low muscle tone, these simple actions can be a source of immense frustration.
Here are a few examples:
- Getting Dressed: Buttoning a shirt, zipping up a coat, or tying shoelaces all require precise finger dexterity and hand strength that might be underdeveloped.
- Mealtime: Just holding a fork correctly, cutting food, or even chewing tougher foods can be a real struggle due to weak muscles in the hands and jaw.
- Personal Hygiene: Squeezing toothpaste onto a brush and holding it steady is another one of those tasks that demands fine motor skills.
Recognizing these real-world impacts is the first step toward providing the right kind of support. It helps validate what you're seeing as a parent and shifts the focus from what your child won't do to what they find physically hard to do. This shift in understanding is the key to creating an environment that supports their academic, social, and emotional needs all at once.
Proven Therapies That Build Strength and Confidence
When it comes to managing autism low muscle tone, the goal isn't to find a "cure." It's about building a strong, functional foundation that helps a child move through their world with greater ease and confidence. A strategic mix of therapies can make a massive difference, helping your child develop strength, coordination, and a sense of accomplishment. These approaches are almost always play-based, targeting specific developmental needs in a way that feels like fun, not work.
The whole point is to help their nervous system and muscles learn to communicate and work together more efficiently. This usually involves a dedicated team of specialists, each focusing on a different—but deeply connected—piece of the motor function puzzle.
Physical Therapy: The Foundation of Strength
Physical Therapy (PT) is often the first and most critical step for a child with hypotonia. Think of a physical therapist as a personal trainer for your child’s developing motor skills. Their main job is to build the core strength needed for just about everything else.
The focus is squarely on strengthening the large muscle groups in the trunk, hips, and shoulders. This provides the stability a child needs to hold their body upright, maintain good posture, and execute coordinated movements.
A PT session often looks just like playtime, but every single activity is chosen with a specific goal in mind:
- Obstacle Courses: Climbing over pillows or crawling through tunnels isn't just fun—it builds core strength and improves motor planning.
- Balance Activities: Walking on a low beam or trying to stand on one foot challenges balance and strengthens all those tiny stabilizing muscles.
- Ball Exercises: Sitting on a large therapy ball or playing catch is a fantastic way to engage core muscles dynamically.
Occupational Therapy: Skills for Daily Life
If PT builds the strong foundation, Occupational Therapy (OT) helps a child use that strength for all the practical, everyday tasks that make up life. OT is all about fine motor skills—those precise, coordinated movements of the hands and fingers needed for getting dressed, eating, and succeeding in school. An occupational therapist bridges the gap between raw strength and functional independence.
Their work centers on activities that improve hand-eye coordination, grip strength, and dexterity. This might look like:
- Playing with therapy putty or clay to strengthen hand muscles.
- Using tweezers to pick up small beads, which refines the pincer grasp.
- Practicing with dressing boards that have buttons, zippers, and snaps.
Therapies for low muscle tone are most effective when they're consistent and woven into a child’s daily routine. The progress made in a therapy session is supercharged by playful reinforcement at home, turning everyday activities into powerful opportunities for growth.
Speech Therapy: Supporting Oral-Motor Skills
It's easy to overlook, but the muscles in our face, jaw, and tongue have "tone" too. For a child with hypotonia, weak oral-motor muscles can cause real trouble, affecting everything from speech clarity to the ability to chew and swallow safely.
Speech-Language Pathologists (SLPs) step in to strengthen these muscles. Their sessions might involve fun exercises like blowing bubbles, drinking thick smoothies through a straw, or making silly, exaggerated facial expressions to build muscle control and coordination.
Take a look at this chart—it really highlights how much extra help kids with autism and low muscle tone often need with key daily tasks.
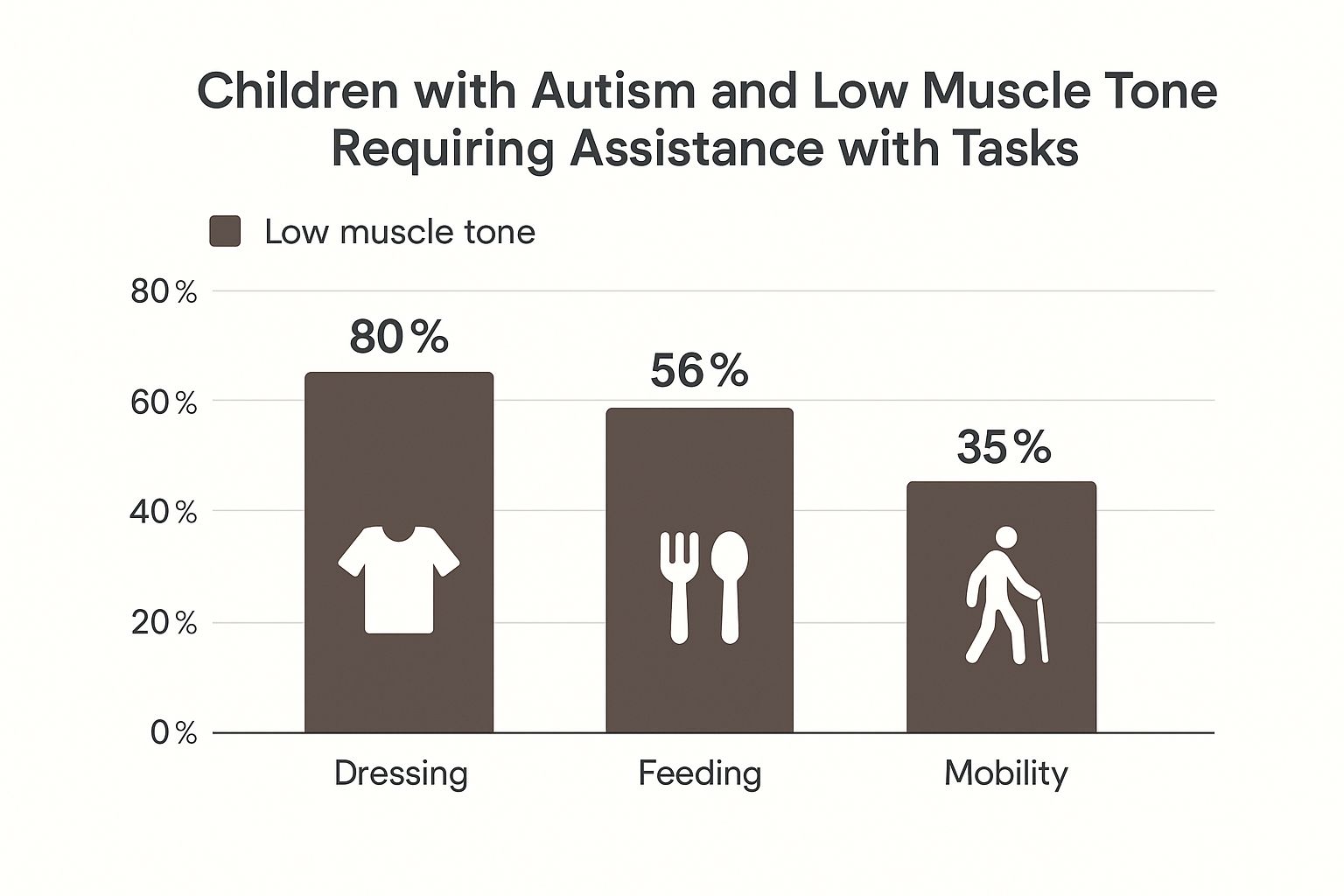
As the data shows, dressing and mobility are major hurdles. This underscores just how vital targeted OT and PT are for building the skills needed for greater independence.
To help you see how these therapies fit together, here’s a quick comparison of their roles in managing low muscle tone.
Comparing Therapeutic Approaches for Low Muscle Tone
| Therapy Type | Primary Focus Area | Example Activities | Key Benefits |
|---|---|---|---|
| Physical Therapy (PT) | Gross motor skills, core strength, balance, and coordination. | Obstacle courses, ball exercises, balancing beams, climbing. | Improved posture, stability, walking, and running. |
| Occupational Therapy (OT) | Fine motor skills, daily living activities, sensory integration. | Using tweezers, playing with putty, buttoning/zipping, writing. | Better self-care skills, handwriting, and tool use. |
| Speech Therapy (SLP) | Oral-motor skills, articulation, feeding, and swallowing. | Blowing bubbles, straw drinking, facial exercises, chewing practice. | Clearer speech, safer eating, improved communication. |
Each therapy brings a unique and essential piece to the puzzle. While PT builds the foundational strength, OT teaches how to use that strength in meaningful ways, and SLP ensures the crucial muscles for communication and eating are also supported. Together, they create a comprehensive support system that empowers a child to thrive.
Simple Ways to Support Motor Skills at Home
You don’t need a home gym or a bunch of expensive equipment to support your child's motor development. In fact, by creatively weaving therapeutic activities into your daily routines, you can turn your home into the perfect environment for building strength and coordination.
The trick is to make it feel like play, not work. Simple, fun activities can have a massive impact on a child with autism low muscle tone. For instance, building a living room obstacle course with pillows to climb over and blankets to crawl under is a fantastic way to engage core muscles and improve motor planning. This kind of play builds the foundational strength they need for better posture and balance.
Fun Activities for Stronger Hands
Fine motor skills also benefit hugely from playful practice. Strengthening those small muscles in the hands is absolutely crucial for everyday tasks like writing, buttoning a shirt, or using a fork.
You can easily mix these activities into your day:
- Play-Doh or Putty: Squeezing, rolling, and pinching therapy putty is an excellent—and fun—hand strengthener.
- Building Blocks: LEGOs and other building toys are amazing for encouraging a precise pincer grasp and improving hand-eye coordination.
- Kitchen Helper: Let them help you stir thick batter or knead dough. It’s a great way to build wrist and hand strength without them even realizing it.
Small Adjustments with Big Impact
Sometimes, the simplest changes are the ones that make the biggest difference. Providing the right kind of support can reduce fatigue and frustration, which allows your child to participate more fully and happily in activities.
Supportive seating, like a small stool under their feet at the dinner table, can provide the stability needed to improve focus and fine motor control. It grounds them, freeing up mental energy that was being used just to stay balanced.
Think about using adaptive tools, like specialized pencil grips that make writing more comfortable or utensils with built-up handles that are easier to hold. These adjustments help bridge the gap while they continue to build that underlying strength.
By combining these supportive strategies with consistent, play-based exercises, you can become an incredible partner in your child's progress. To learn more about building a strong foundation, check out our guide on how to strengthen core muscles.
Common Questions About Autism and Low Muscle Tone
When you’re navigating the world of autism low muscle tone, it’s completely normal to have a lot of questions. We’ve put together this quick guide to address the most common concerns we hear from parents, giving you clear, reassuring answers to feel more confident and informed.
Can My Child's Low Muscle Tone Improve Over Time?
Yes, absolutely. While hypotonia is often a lifelong condition tied to the unique neurology of autism, it can be significantly managed and improved.
Targeted therapies like physical and occupational therapy are designed to build functional strength, better coordination, and endurance. The goal isn’t to "cure" low muscle tone but to help your child's brain and muscles learn to communicate more efficiently. With consistent support, children can make incredible progress in their motor skills, which leads to greater independence and confidence in daily life.
Is Low Muscle Tone the Same as Muscle Weakness?
This is a great question, and it’s one we hear all the time. The two are closely related, but they aren't the same thing.
Low muscle tone (hypotonia) is all about the amount of tension in a muscle when it’s at rest. If a child has hypotonia, they might feel a bit "floppy" when you hold them. Muscle weakness, on the other hand, is about a muscle's ability to actually generate force and do work.
A child with low tone often has muscle weakness because it takes so much more effort to activate their "sleepy" muscles to perform a task. Most therapies will address both issues at once, building underlying strength while also improving motor control.
What Should I Do First if I Suspect My Child Has Hypotonia?
The best first step is always to schedule an appointment with your child's pediatrician. Before you go, jot down some specific observations about their posture, movements, and any delays in motor skills you've noticed. This will be incredibly helpful during your visit.
Your pediatrician can perform an initial assessment. If they share your concerns, they will likely provide a referral to a specialist, like a developmental pediatrician, or send you directly to physical and occupational therapists for a more comprehensive evaluation. Getting an assessment early is the key to getting your child the right support as soon as possible.
At First Steps Chiropractic, our focus is on optimizing nervous system function to better support children with developmental challenges. If you're exploring ways to help your child thrive, we invite you to learn more about our gentle, neurologically-focused approach.

