If you've ever found yourself staring at the ceiling at 3 AM while your baby cries, you know just how exhausting and lonely it can feel. Every parent has been there, wondering if the constant waking is just a phase or a sign of something more.
That uncertainty can be overwhelming. It’s tough to tell the difference between normal developmental hiccups and the potential signs of genuine infant sleep disorders. You are not alone in this, and finding a solution starts with understanding the problem.

This guide is designed to give you some immediate reassurance and a clear roadmap forward. We'll help you navigate the confusion, starting with a simple framework to understand the "why" behind your baby's sleep challenges. When we frame these issues as a common but manageable part of parenting, it empowers you with the knowledge to take the next step.
So, what exactly are infant sleep disorders? Simply put, they are medical conditions that get in the way of a baby's ability to fall asleep, stay asleep, or get truly restful sleep. While many sleep issues are just part of growing up, a true disorder involves persistent patterns that impact your baby's health and your family's well-being, often requiring a professional look.
Normal Sleep Patterns vs. Potential Red Flags
The very first step in identifying a potential problem is knowing what's typical for a baby. Infant sleep isn't a straight line—it's more like a winding path with regressions, growth spurts, and developmental leaps that all mess with rest.
Think of it like this: a fussy evening before a growth spurt is like a brief rain shower. It’s expected and temporary. But nightly struggles that include gasping for air or extreme, inconsolable crying are more like a persistent storm that signals it’s time to check the forecast.
A key distinction lies in frequency, intensity, and impact. While occasional night wakings are normal, consistent, severe disruptions that affect your baby's daytime mood, feeding, or growth may indicate an underlying issue.
To help you tell the difference, let’s quickly compare what's generally considered normal with signs that might point to a bigger issue.
Normal Infant Sleep Patterns vs Potential Disorder Signs
This table is a quick guide to help you differentiate between typical baby sleep behaviors and red flags that may point to an underlying sleep disorder.
| Age Range | Typical Sleep Behavior | Potential Red Flags to Watch |
|---|---|---|
| 0-3 Months | Irregular sleep-wake cycles, waking every 2-4 hours to feed, active sleep with twitching/grunting. | Extreme fussiness for hours (colic), difficulty being soothed, poor weight gain, choking or gasping during sleep. |
| 4-7 Months | Sleep cycles start to lengthen, potential 4-month sleep regression, may wake 1-3 times per night. | Consistent inability to self-soothe, frequent night wakings not related to hunger, loud or persistent snoring. |
| 8-12 Months | May experience another regression due to separation anxiety or new skills (crawling, pulling up), usually wakes 0-2 times. | Night terrors (screaming while asleep), significant pauses in breathing (apnea), still waking every 1-2 hours. |
Remember, this is just a starting point. Every baby is different, but this can help you spot patterns that feel outside the norm.
To give you a bit more context, here are a few key things to consider:
- Developmental Hurdles: Sleep regressions around 4, 8, and 12 months are totally normal. These are just temporary setbacks caused by your baby learning cool new skills like rolling over or crawling.
- Physical Discomfort: Things like teething, gas, or reflux can definitely disrupt sleep for a bit. These issues are usually tied to a specific cause and get better once the discomfort is managed.
- Behavioral Patterns: Sometimes, a baby just gets used to being rocked or fed to sleep. While this can be challenging for you, it’s a habit, not necessarily a disorder.
- Concerning Symptoms: This is the important one. Persistent, loud snoring, choking or gasping sounds, or noticeable pauses in breathing are significant red flags that need medical attention.
By learning to separate these categories, you can get a much clearer picture of your situation. This guide will walk you through the specifics of each, giving you the confidence to support your baby’s sleep and know exactly when it’s time to seek professional help for potential infant sleep disorders.
Identifying Common Infant Sleep Disorders
Moving from worry to clarity all starts with knowing what you’re looking for. It's true that many infant sleep troubles are just normal developmental phases they have to go through. But sometimes, persistent patterns can point toward a specific infant sleep disorder.
Think of it less like a scary medical diagnosis and more like finding the right key for a stubborn lock. Once you know exactly what you’re up against, you can find the right solution to help everyone get some rest.
The most common issues usually fall into a few main categories. Many are behavioral, meaning they’re tied to sleep associations and routines. Others are physiological, stemming from how a baby's body is actually functioning during sleep. Let's break down what you're most likely to see.
This visual guide breaks down the main categories of infant sleep disorders, helping you see how different issues like sleep apnea and frequent night wakings are classified.
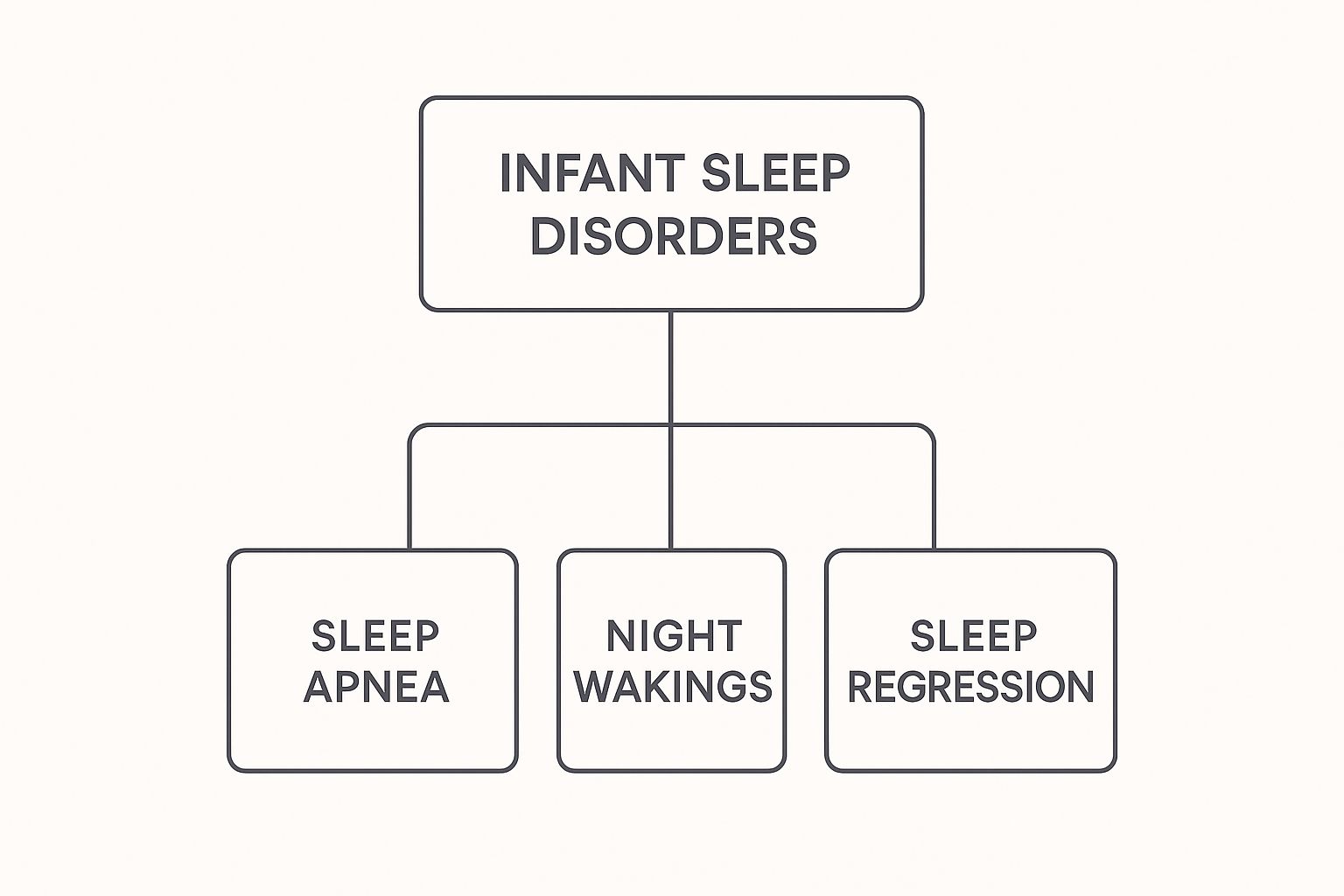
This hierarchy shows that while issues like sleep regression are common concerns, they are distinct from medical conditions such as sleep apnea that require a different level of attention.
Behavioral Insomnia of Childhood
This is one of the most frequent challenges parents face. It isn't really about a baby's inability to sleep, but more about the conditions they’ve learned to associate with falling asleep. You’ll probably recognize one of these two types.
- Sleep-Onset Association Type: Does your baby only fall asleep while being rocked, fed, or held? If so, when they naturally wake up between sleep cycles at night, they need that exact same condition to get back to sleep. This isn't manipulation; it’s simply a learned dependence.
- Limit-Setting Type: This is more common with toddlers but can definitely start in late infancy. It’s what happens when a baby or child resists bedtime with protests, demands, or "curtain calls," usually because the boundaries around the bedtime routine are a bit fuzzy or inconsistent.
These behaviors are almost always rooted in routine. For example, if a baby is always nursed to sleep, their brain forges a powerful link: "food" equals "sleep." When they stir in the night and find themselves alone in their crib, the absence of that comfort is jarring, and they’ll cry until the association (nursing) is offered again.
Sleep-Related Breathing Disorders
This category is a crucial one because it directly involves a baby’s physical health. The most well-known condition here is Obstructive Sleep Apnea (OSA).
Picture a very soft, flexible drinking straw. If you try to suck through it and it collapses on itself, air can't get through. An infant's airway is naturally small and floppy, just like that straw. During sleep, their muscles relax, and for some babies, the airway can partially or completely collapse, which blocks airflow.
While an estimated 1-5% of all children experience OSA, the signs in infants can be incredibly subtle. It's more than just soft snoring; it's about the quality of their breathing while they rest.
Key signs of potential sleep apnea to watch for include:
- Loud, persistent snoring: We’re not talking about little grunts, but noisy breathing that happens most nights.
- Gasping or choking sounds: You might hear them suddenly gasp for air after a brief pause in their breathing.
- Noticeable pauses in breathing: These are the most significant red flags.
- Restless sleep: Frequent tossing and turning, or sleeping in odd positions (like with their neck arched way back) in an attempt to open their airway.
These breathing disruptions lead to poor-quality, fragmented sleep that can impact everything from their mood to their physical growth.
Parasomnias and Circadian Rhythm Disorders
These infant sleep disorders are less common, but they're still important to have on your radar. Parasomnias are disruptive events that happen during sleep, like sleepwalking or night terrors. While they’re more common in older kids, early signs can sometimes show up in infancy as unusual or dramatic night wakings.
Circadian Rhythm Disorders happen when a baby's internal body clock gets out of sync with our 24-hour day. This might lead to a delayed sleep phase, where they consistently fall asleep and wake up much later than is typical.
While most newborns have chaotic schedules at first, a persistent and unmovable pattern could point to a circadian issue. Sometimes, these sensitivities to routine and environment can overlap with other challenges; you can learn more about sensory issues in infants to see how they connect to overall comfort and regulation.
Creating a Safe Sleep Environment
Knowing about infant sleep disorders is one side of the coin. The other, equally important side, is making sure the physical space where your baby sleeps is as safe as it can possibly be.
This topic can feel heavy, and it often brings up scary terms like Sudden Unexpected Infant Death (SUID) and its most well-known type, Sudden Infant Death Syndrome (SIDS).

It’s so important to approach this with empowerment, not fear. SUID and SIDS aren't caused by a parent missing something or making a mistake. They are incredibly complex and often involve a combination of factors—some of which we can directly influence by creating a safer sleep environment.
Our goal here is to give you clear, evidence-based steps to dramatically reduce risks. We want you to feel confident and secure every single time you lay your baby down to rest.
The ABCs of Safe Sleep
The easiest way to remember the core rules of safe sleep is the acronym ABC: Alone on their Back in a Crib. This simple guideline is the bedrock of infant sleep safety and has been proven to save lives.
Let’s unpack exactly what each part means for you and your baby.
- A is for ALONE: Your baby needs their own separate space, like a crib, bassinet, or play yard. Nothing else should be in there with them—no blankets, no pillows, no crib bumpers, no stuffed animals, and no loose bedding. All of these items, however cute, pose a serious suffocation risk.
- B is for BACK: Always, always place your baby on their back for every single sleep, whether it’s a quick nap or for the night. A baby’s airway is best protected in this position. Once they are strong enough to consistently roll from their back to their tummy and back again all by themselves, you don’t have to keep flipping them over.
- C is for CRIB: The sleep surface itself is a huge factor. It must be a firm, flat mattress made specifically for that crib or bassinet, covered only with a tight-fitting sheet. Soft surfaces like an adult bed, a couch, or an armchair are dangerous and increase the risk of accidental suffocation.
Following these ABCs is the single most powerful action you can take to create a safe sleep space and lower the risks associated with many infant sleep challenges.
Room-Sharing Without Bed-Sharing
While your baby should be alone in their crib, that doesn't mean they have to be in another room. In fact, the American Academy of Pediatrics recommends room-sharing for at least the first six months, and ideally for the whole first year.
Keeping your baby’s crib or bassinet right in your room, close to your bed, makes those middle-of-the-night feedings and comfort sessions so much easier. More importantly, research has shown this practice can reduce the risk of SIDS by as much as 50%. You get all the protective benefits of being close without the real dangers that come with bed-sharing.
Bed-sharing, which means having your baby sleep in the same bed with you, significantly increases the risk of accidental suffocation, strangulation, and entrapment. This is especially true for infants under four months old. A separate, safe sleep space is always the best choice.
Understanding the Statistics and Reducing Risks
Public health campaigns pushing these safe sleep practices have made a huge difference. In the United States, SUID rates dropped from 158.58 deaths per 100,000 live births in 1990 down to 92.9 deaths per 100,000 in 2020. That's real progress.
However, a review of SUID cases found that a staggering 46% involved bed-sharing, and only 34.5% of the infants had been placed on their backs to sleep. This just goes to show how vital it is that we continue to get this information out there.
Sometimes, discomfort from issues like colic can make these guidelines feel impossible to follow. A fussy baby might only seem to settle in an unsafe position or on a soft surface. If you're struggling with an inconsolable infant, exploring gentle ways to provide comfort is key. Finding effective strategies for colic relief for newborns can help soothe your baby, making it much easier to stick to safe sleep practices.
Creating a safe sleep environment is all about layering these protective factors to give your child the safest start possible.
Why Consistent Sleep Is a Developmental Superpower
Sleep is so much more than a quiet break for exhausted parents; it's the invisible architect of your baby’s development. You can think of it like a master construction crew that works the night shift. While your baby is busy absorbing a flood of new sights, sounds, and sensations all day, sleep gets to work organizing all that information, building and reinforcing the very foundation of their future.
While your baby rests, their brain is incredibly active. It’s busy solidifying memories, forging critical neural connections, and even practicing new motor skills. Every single hour of uninterrupted sleep is a powerful investment in their cognitive, emotional, and physical growth. This is the time when the building blocks for learning, mood regulation, and physical coordination are firmly set in place.
The Brain-Building Power of Uninterrupted Sleep
Imagine your baby’s brain is like a bustling library. During the day, new books—which are their experiences and memories—are constantly arriving and being piled up near the entrance. It's during sleep that the librarians meticulously sort through each book, cataloging it and placing it on the correct shelf. Without this nightly organization, the library would quickly become a chaotic mess, making it difficult to find anything.
Fragmented or poor-quality sleep interrupts this vital process. When an infant sleep disorder constantly disrupts rest, those "librarians" never get a chance to finish their work. This is why consistent, restorative sleep is so critical for:
- Memory Consolidation: Helping your baby remember faces, routines, and newly learned skills like clapping or waving.
- Neural Pathway Formation: Strengthening the connections that support everything from language development to problem-solving later in life.
- Emotional Regulation: Giving the brain time to process emotions, which helps your baby wake up happier and better able to handle stimulation.
A well-rested baby isn't just less fussy; they are actively building a healthier, more resilient brain. Quality sleep is the fuel for their developmental engine.
The Ripple Effect of Poor Sleep on Development
When sleep is consistently disrupted by infant sleep disorders, the consequences go far beyond just being tired. Sleep disturbances in infancy carry significant developmental risks that can have a lasting impact.
Children who experience inadequate or fragmented sleep face increased risks of cognitive impairment, behavioral problems, and delayed learning. In fact, research shows that irregular sleep patterns are directly linked to heightened behavioral issues and suboptimal developmental outcomes. You can read more about these infant sleep findings on nature.com.
This table breaks down exactly how different areas of development are impacted by sleep quality.
How Healthy Sleep Fuels Infant Development
| Developmental Area | Benefits of Healthy Sleep | Risks of Poor Sleep |
|---|---|---|
| Cognitive Function | Improved learning, memory recall, and attention span. | Difficulty focusing, delayed language skills, and learning challenges. |
| Emotional Health | Better mood, increased resilience to stress, and easier self-soothing. | Increased irritability, fussiness, and difficulty regulating emotions. |
| Physical Growth | Release of growth hormone, muscle repair, and a stronger immune system. | Slower weight gain, weakened immunity, and impaired motor skill development. |
Viewing sleep through this lens really shifts your perspective. Establishing healthy sleep habits isn't just a short-term solution for your own sanity. It's a foundational, long-term investment in your child’s lifelong well-being.
Global Lessons in Infant Sleep Safety
The safe sleep advice you hear today didn't just appear out of thin air. It's the result of decades of global research and some hard-won lessons from families and healthcare professionals all over the world. When you step back and look at the bigger picture, you can see just how powerful these simple, science-backed recommendations truly are.
The data tells a compelling story, one of incredible public health success. But it also shines a light on the work we still have to do to protect every single baby, no matter where they live.

This global view isn't just an academic exercise—it’s solid proof that clear, consistent messaging saves lives. It helps us appreciate that every time we create a safe sleep space for our little ones, we're part of a massive, worldwide effort to prevent tragedy and support healthy infant development.
The Worldwide Impact of Back to Sleep
Back in the early 1990s, countries around the globe kicked off major public health campaigns. The most famous one was "Back to Sleep," which we now know as Safe to Sleep®. The message was incredibly simple but had a profound impact: place babies on their backs for every single sleep.
The results were nothing short of remarkable. This single, coordinated effort led to a huge drop in the rates of Sudden Infant Death Syndrome (SIDS), one of the most heartbreaking infant sleep disorders. Between 1990 and 2021, the worldwide rate of SIDS fell by an incredible 59%. That statistic is a powerful testament to how effective these campaigns were. You can discover more about these global SIDS trends to see the full impact.
This success story proves that straightforward, evidence-based guidance isn't limited by borders or cultures. The "ABCs of Safe Sleep" aren't just a local tip; they're a global standard built on a mountain of solid scientific evidence.
Understanding Global Disparities in Sleep Safety
Even with this incredible progress, the story of infant sleep safety isn't the same everywhere. Big differences still exist from one community to another, often tied to things like socioeconomic status, cultural traditions, and access to good healthcare and education. It’s a clear reminder that knowledge isn't always enough; families need support systems and resources, too.
For instance, while SIDS rates have plummeted in many developed nations, some regions still face significant struggles. The highest SIDS rate is currently in Western Sub-Saharan Africa, which saw 46.6 deaths for every 100,000 infants in 2021. This number shows how factors like poverty, limited prenatal care, and different cultural norms around infant sleep can create real barriers to putting safe practices into place.
Several things contribute to these global disparities:
- Socioeconomic Conditions: Families with low incomes might not have access to a safe crib, or they might live in crowded homes where bed-sharing feels like the only practical choice.
- Cultural Practices: Some traditional ways of caring for infants, like co-sleeping or using soft, plush bedding, can conflict with modern safe sleep guidelines.
- Healthcare Access: Without consistent prenatal and postnatal care, many parents may never get the crucial education they need about creating a safe sleep environment.
Acknowledging these global challenges doesn't weaken the safe sleep message—it makes it stronger. It reminds us that every family deserves the education, resources, and support needed to provide the safest possible sleep environment for their child.
Ultimately, the global fight against infant sleep disorders and unsafe practices shows us what’s possible when science, public health, and parents all come together. It’s a powerful reminder that every time you place your baby alone, on their back, in a crib, you're part of a worldwide movement that has saved countless lives.
You've tried everything. You’ve established a solid routine, created the perfect sleep sanctuary, and followed all the best advice. But your baby’s sleep challenges just won’t budge, and you’re left feeling completely exhausted and helpless.
Knowing when to move from home-based strategies to professional support is a huge, and often difficult, step. But this isn't about admitting defeat. It's a sign of your strength as a parent and a proactive move to protect your child’s health and well-being.
Recognizing Red Flags
As a parent, your intuition is one of your most powerful tools. If you have a gut feeling that something is just “off” with your baby’s sleep, it’s always worth looking into. Persistent issues that don’t get better with time or a consistent routine are often a sign that there's an underlying factor that needs a closer look.
Certain symptoms go way beyond typical fussy baby stuff and should absolutely prompt a conversation with your pediatrician. Think of these as clear signals that your baby’s body is asking for help.
Pay close attention if you notice any of these patterns:
- Breathing Irregularities: This one is the most urgent. Loud, habitual snoring, gasping for air, or noticeable pauses in breathing while sleeping are major red flags that need immediate medical attention.
- Poor Weight Gain or Feeding Issues: Healthy sleep and healthy growth go hand-in-hand. If your baby is struggling to gain weight, seems unusually sleepy during feedings, or has a hard time coordinating sucking and breathing, it could be tied to poor-quality sleep.
- Extreme Irritability or Inconsolability: All babies get fussy, but persistent, high-pitched crying or extreme difficulty being soothed can sometimes point to discomfort from an underlying sleep issue.
- Consistently Poor Sleep Quality: If your baby is an extremely restless sleeper, frequently arches their back in discomfort, or always seems to wake up just as tired as they were when they fell asleep, it’s time for a professional evaluation.
Seeking professional help is a proactive step toward ensuring your child's optimal development. Addressing sleep issues early can prevent them from impacting other areas, such as cognitive function and emotional regulation.
What to Expect During the Diagnostic Process
Bringing up your concerns with a doctor might feel a little intimidating, but it’s a partnership. Your pediatrician is on your team and will likely start by gathering a detailed sleep history. They’ll want to know all about your bedtime routines, night wakings, feeding schedules, and the specific symptoms you've been seeing.
From there, the process might involve a few next steps:
- A Thorough Physical Examination: Your doctor will check for physical signs that could explain the sleep disruptions, like enlarged tonsils or other anatomical issues.
- Keeping a Sleep Diary: You might be asked to log your baby’s sleep patterns for a week or two. This gives your doctor a clear, detailed picture of what's really going on.
- Referral to a Specialist: If an infant sleep disorder like obstructive sleep apnea is suspected, you’ll likely be referred to a pediatric sleep specialist or an ENT (otolaryngologist) for more evaluation. Sometimes, addressing related neurological stress can also be a key piece of the puzzle; you can learn more about how chiropractors can support children with autism and similar neuro-developmental challenges.
Your Top Questions About Infant Sleep, Answered
Trying to understand your baby's sleep patterns can feel like a guessing game, leaving you with more questions than answers. Even after you've learned the basics, some worries can linger.
We've pulled together some of the most common questions we hear from parents to give you clear, straightforward answers and help you feel more confident on your journey to better sleep.
Can Sleep Training Cause an Infant Sleep Disorder?
This is a big worry for many parents, but let's clear the air: when done safely and at the right age, sleep training does not cause sleep disorders. Its goal is to teach healthy sleep habits and self-soothing skills, not to create underlying medical problems like sleep apnea.
However, it's a different story if your baby has an undiagnosed issue like reflux or breathing trouble. In that case, sleep training won't work and will only add stress for everyone. It's always a good idea to chat with your pediatrician to rule out any medical concerns before you start a new sleep plan.
How Can I Tell if My Baby's Snoring Is a Problem?
Not all baby snores are created equal. Those soft, little grunts and occasional snores are usually perfectly normal. A newborn's airway is tiny and still developing, so some noise is expected.
The time to pay closer attention is when the snoring is loud, consistent, and happens almost every night. If you also hear gasping, choking sounds, or see long pauses in their breathing, it's a definite sign to call your pediatrician. These can be indicators of obstructive sleep apnea, a serious infant sleep disorder that needs a proper evaluation.
Think of it like this: a soft little purr is one thing, but a loud, rattling engine is a clear signal that something needs a check-up.
Are Night Terrors the Same as Nightmares?
It's easy to confuse them, but they are very different, and knowing why can bring a lot of peace of mind.
- Nightmares are just bad dreams. They usually happen in the later part of the night, and your child will wake up genuinely scared. They'll know who you are and will want comfort, which usually helps them settle back down.
- Night Terrors are a whole other ballgame. These are episodes, not dreams, that happen during deep sleep, often just a few hours after bedtime. Your child might scream, thrash, or look terrified, but they are completely asleep and won't recognize you. The next day, they won't remember a thing.
While they look incredibly scary for the parent watching, night terrors aren't harmful and are something most kids outgrow. The best you can do is stay nearby to make sure they're safe and let the episode run its course.
At First Steps Chiropractic, we know that when your baby sleeps well, the whole family thrives. If you're struggling with sleep challenges that just won't go away, our neurologically-focused care can help uncover and address the underlying nervous system stress that might be getting in the way. Learn more about our gentle, effective approach for infants and families at https://firststepschiropractic.com.