When you hear "stem cell therapy," what comes to mind? For a growing number of people dealing with chronic pain, it represents hope—a real chance to heal from the inside out. This approach uses your body's own remarkable healing abilities to repair damaged tissue and calm inflammation right at the source.
Instead of just masking symptoms, this regenerative method gets to the root cause of the problem. It’s a completely different way of thinking about what recovery can and should look like.
A Modern Answer to Chronic Pain

Living with chronic pain is like being stuck in a frustrating loop. Every day is a gamble, governed by stiffness, limited mobility, and the constant question of whether you can get through simple tasks without a flare-up. You've probably been down the usual road: pain medications, physical therapy, maybe even steroid injections. But the relief never seems to last.
This path feels a lot like putting a bucket under a leaky roof. Sure, it manages the immediate mess, but it does absolutely nothing to fix the hole.
The real frustration kicks in when you realize these methods are designed to manage symptoms, not solve the underlying problem. Painkillers might give you a few hours of peace, but they can't repair the worn-out cartilage in your knee or the torn tendon in your shoulder. This reactive cycle leaves so many people feeling stuck and searching for something that actually promotes healing.
Shifting from Symptom Management to True Healing
This is where regenerative medicine, and specifically stem cell therapy for pain, changes the game. It moves the focus away from simply managing symptoms and toward rebuilding and restoring damaged tissue from within. Instead of just trying to silence the pain signals, it helps your body fix what’s causing them in the first place.
This is a major shift in how we approach pain. The goal is no longer just making the pain tolerable; it's about improving function and getting your quality of life back. Think about being able to walk, run, or play with your kids without that constant, familiar ache holding you back. That's the real promise of working with your body's own healing potential.
At its core, stem cell therapy is about cooperation with the body's natural healing systems. It provides the essential biological tools—the cells—that are needed to kickstart a repair process that may have stalled due to age, injury, or chronic inflammation.
Comparing Old and New Approaches
To really see the difference, it helps to put the two philosophies side-by-side. Traditional treatments certainly have their place, but they operate on a completely different principle than regenerative medicine.
Traditional Pain Management vs. Regenerative Medicine
Take a look at how these two approaches stack up. It becomes clear why so many are looking for a new way forward.
| Aspect | Traditional Treatments (e.g., Medication, Surgery) | Stem Cell Therapy |
|---|---|---|
| Primary Goal | Symptom suppression and management of pain signals. | Tissue repair and resolution of the underlying cause. |
| Mechanism | Blocks pain pathways or surgically removes damaged tissue. | Reduces inflammation and regenerates damaged cells. |
| Duration of Effect | Often temporary, requiring ongoing treatment. | Aims for long-term, lasting structural improvement. |
| Approach | Often reactive, addressing pain after it becomes severe. | Proactive, focused on healing to prevent further decline. |
This comparison really highlights why regenerative options are gaining so much attention. For anyone tired of temporary fixes, understanding how stem cell therapy for pain works is the first step toward a path of genuine, lasting recovery.
How Stem Cells Get to the Root of Your Pain
To really get how stem cell therapy works, let's use an analogy. Think of your body as a construction project. An injury, like worn-out cartilage in your knee, is like a critical support beam developing a crack. Your body sends out a distress signal, but sometimes the local repair crew is just too overwhelmed or doesn't have the right materials for the job.
Stem cells are the elite, specialized repair team called in to fix the problem right. They don't just slap a patch on the crack; they rebuild the beam from the inside out. They're addressing the fundamental structural issue that’s causing all the instability and pain in the first place.
And that's the real difference between regenerative medicine and just masking symptoms.
These incredible cells work in two key phases. First, they act as powerful anti-inflammatory agents to calm the chaos at the injury site. That brings some initial relief, but their most important work is still to come.
The Anti-Inflammatory Response
Imagine that cracked beam has now caught fire—that's inflammation. It’s chaotic, destructive, and makes it impossible for any real repair work to get started. The very first thing the fire department does is put out the flames.
Stem cells do something very similar. Once they arrive at the damaged tissue, they release proteins called cytokines. Think of these molecules as a potent fire extinguisher, signaling the body's overactive immune response to stand down and calm down.
This process is what reduces swelling, heat, and pain. By quieting the inflammation, stem cells create a stable environment where the real healing and rebuilding can finally begin. It’s a crucial first step that shifts the body from a state of chronic irritation to one of active repair.
This initial anti-inflammatory effect is why some people feel better pretty quickly. It's the first clear sign that your body is shifting gears from a cycle of damage to a process of recovery, laying the groundwork for deeper, more lasting healing.
The Regenerative Mission
With the "fire" of inflammation under control, the stem cells can now get to their main job: rebuilding. This is where their unique ability, called differentiation, shines. Stem cells are like biological blank slates, capable of transforming into the exact type of specialized cell the body needs to heal.
So, if your pain is from a knee with worn-down cartilage, stem cells can become new cartilage cells (chondrocytes). If a shoulder tendon is torn, they can become new tendon cells (tenocytes). They essentially read the biological blueprints of the damaged area and start filling in the missing pieces with fresh, healthy tissue.
This targeted regeneration gets right to the root cause of the pain. It’s not about masking discomfort; it’s about fixing the mechanical failure that created it in the first place. By restoring the integrity of the joint or soft tissue, stem cell therapy for pain offers a genuine path toward long-term functional improvement.
The whole process unfolds in a few key steps:
- Homing: Stem cells are naturally drawn to the chemical signals of distress and inflammation your body sends out. When introduced, they navigate directly to the site of the injury.
- Signaling: Once they arrive, they communicate with surrounding cells, essentially directing the repair process and calling for additional healing support from the body.
- Differentiation: This is the transformation. The stem cells become the specific cell type needed—cartilage, bone, tendon, or ligament—to rebuild the damaged structure.
- Tissue Integration: Over the following weeks and months, this new tissue integrates with the existing structure, strengthening the area and helping restore its normal function.
By following this intelligent, natural process, stem cells don't just manage pain—they empower your body to heal itself in a way it couldn't do on its own.
What Conditions Respond Best to Stem Cell Therapy
Now that we've covered how stem cells do their thing, the big question is: where do they work best? While the potential is huge, stem cell therapy for pain really shines in specific areas where chronic inflammation and tissue damage are the main problems.
Think of it like calling in a specialist for a very specific job. This therapy gets the best results when we target conditions caused by wear-and-tear or an old injury where the body’s own repair crew just couldn't keep up.
These conditions typically fall into a couple of key categories: degenerative joint diseases and soft tissue injuries that just won’t heal right. In both cases, the mission is the same: repair the underlying damage, quiet down the inflammation, and get you moving again.
Joint Pain and Osteoarthritis
Osteoarthritis (OA) is probably the most common reason people look into stem cell therapy. It’s the classic "wear and tear" arthritis, where the smooth cartilage cushioning your joints starts to break down over time.
Picture the slick, gliding surface inside a healthy joint becoming rough and potholed. That friction is what causes the pain, stiffness, and swelling. Stem cell therapy tackles this head-on by introducing new cells that can help calm the inflammation and potentially signal the body to repair the joint environment.
The most common joints we see respond well are:
- Knees: As the joints that carry most of our weight, knees are prime candidates for OA. Many studies show that stem cell injections can lead to big improvements in pain and mobility.
- Hips: Hip arthritis can be a game-changer, often ending in a total replacement. Regenerative medicine offers a less invasive path to help preserve your natural joint and potentially put off or even avoid that major surgery.
- Shoulders: The shoulder is incredibly complex, and when its cartilage is damaged, your range of motion can become severely limited. Stem cells can get in there to help repair that damage and cool off the constant inflammation.
For so many people living with osteoarthritis, the goal isn't just to stop the pain. It’s about getting back to life—walking the dog, gardening, or playing with the grandkids without that constant, nagging ache.
Soft Tissue and Sports Injuries
It’s not just about joints. Stem cell therapy is also incredibly effective for injuries to muscles, ligaments, and tendons. While these are often called "sports injuries," they can happen to anyone from overuse or just a bad accident.
These tissues don’t get a lot of blood flow, which means healing is slow and often incomplete. Stem cells give your body a helping hand by delivering a powerful concentration of healing signals right where they're needed, kickstarting the repair of torn or worn-out fibers.
Some of the most common soft tissue injuries we see are:
- Rotator Cuff Tears: A tear in those shoulder tendons can cause constant pain and weakness. Stem cell therapy can help rebuild those torn fibers, restoring strength and dialing down the pain.
- Tendonitis: Nagging issues like tennis elbow or Achilles tendonitis are all about chronic inflammation and tiny tears in the tendon. The therapy works to calm that fire and help the tissue finally heal.
- Ligament Sprains: A bad sprain, like one to the ACL in your knee, can leave the joint feeling unstable. Stem cells can help strengthen and repair that damaged ligament to restore stability.
Learning to manage these types of conditions is a key part of any long-term health plan. For more on this, you can read our guide on how to manage chronic pain.
Neuropathic and Nerve-Related Pain
One of the most exciting new frontiers is using stem cells for neuropathic pain—the kind that comes from damaged nerves. This type of pain is famously tough to treat with traditional medicine.
The amount of research into stem cells for nerve pain has exploded over the past few decades. The U.S., China, and Japan are leading the charge, with top institutions like Johns Hopkins and Duke University publishing groundbreaking work. Scientists are digging into exactly how stem cells can influence inflammatory signals, neuropeptides, and other pathways that regulate pain and regenerate tissue.
Navigating Your Stem Cell Treatment Journey
Understanding the science behind stem cell therapy is one thing, but knowing what to expect from the process is another. The idea of any new medical procedure can feel a little intimidating, but the journey is actually quite straightforward. When you break it down into clear stages, you can move forward with confidence instead of uncertainty.
The entire process is a partnership between you and your provider. From the very first conversation all the way through your final follow-up, our goal is to make sure you feel informed, comfortable, and in control.
Let’s walk through what the journey looks like, step by step.
The First Step: Your Initial Consultation
The path to stem cell therapy for pain always starts with a detailed consultation. This is much more than a routine check-up; it’s a deep dive into your health history, the specifics of your pain, and what you’re hoping to achieve. Think of it as a strategy session where we map out your current situation to see if this is the right route for you.
During this visit, we’ll review any existing imaging you have—like MRIs or X-rays—to get a clear picture of the tissue damage. A thorough physical exam also helps us understand your functional limitations. This initial evaluation is crucial for figuring out if you're a good candidate and for setting realistic expectations for your recovery.
The Treatment Day: What to Expect
Once we confirm you’re a good candidate and have a personalized plan in place, the next step is the treatment itself. The procedure is minimally invasive and performed right here in the clinic, usually taking just a couple of hours from start to finish. We design the whole process to be as comfortable as possible.
This infographic breaks down the core steps of a typical procedure.
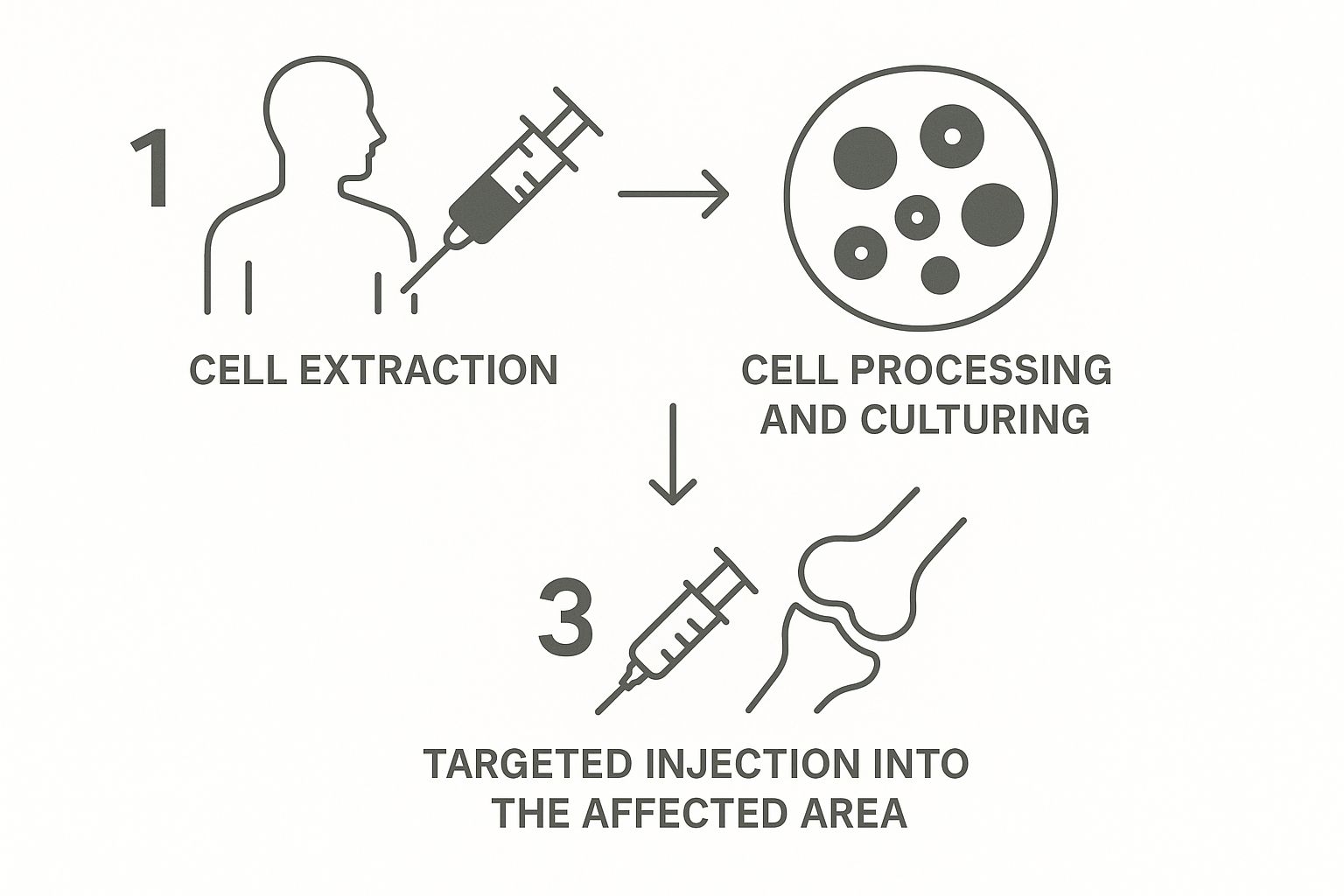
As you can see, the process involves collecting, preparing, and then precisely delivering the regenerative cells to the target area. This is what kickstarts your body’s natural healing cascade.
Recovery and the Healing Phase
After the procedure, the real work begins—inside your body. The recovery phase is when the stem cells go on their anti-inflammatory and regenerative mission. Most people can get back to their normal daily activities within a day or two, but it's important to avoid strenuous exercise for a short period, just as your doctor advises.
It's essential to remember that this is a biological repair process, not a quick fix. While some patients report feeling a reduction in inflammation within a few weeks, the most significant improvements in pain and function typically appear between three to six months as new tissue forms and matures.
This timeline is a testament to genuine healing. Your body is rebuilding itself from the inside out, and that just takes time. We’ll schedule follow-up appointments to monitor your progress and make sure you're healing optimally.
Research continues to back this up. For instance, recent clinical data reported success rates between 50% to 90%, depending on the condition. Some studies even showed a 19% disability improvement in MS patients over five years, compared to just 4% with traditional methods. You can find more details on these promising outcomes in a comprehensive report on stem cell therapy success rates.
Amplifying Healing with SoftWave Therapy
While stem cell therapy is like bringing in a highly specialized construction crew to repair an injury, what if you could also send out a powerful signal to rally your body’s own local healing reserves? This is where complementary therapies like SoftWave can make a world of difference, prepping the tissue for optimal repair.
Think of it this way: if stem cell therapy for pain is the elite repair crew, SoftWave therapy is the emergency broadcast that goes out first. It's a powerful, non-invasive alert that tells your body’s resident stem cells that their help is needed—right now.
This creates a powerful one-two punch for healing. You’re not just relying on the newly introduced cells; you’re also awakening the massive regenerative potential that already exists inside your body.
How SoftWave Wakes Up Your Body's Own Stem Cells
SoftWave therapy uses a special device to send electrohydraulic supersonic acoustic waves deep into injured areas. Don't let the name intimidate you; these aren't electric shocks. They are sound waves that trigger a gentle but profound biological response. This process, called mechanotransduction, essentially shakes dormant cells awake and kickstarts a whole cascade of natural healing activities.
The main benefits of this wake-up call include:
- Stem Cell Activation: The waves signal your body's own resident stem cells to migrate to the targeted area. This boosts the total number of repair cells available to fix the damage.
- Improved Blood Flow: SoftWave stimulates the formation of new blood vessels (a process called angiogenesis). Better circulation is absolutely critical for healing, as it delivers more oxygen and nutrients right where they're needed.
- Reduced Inflammation: The therapy helps calm the inflammatory response, dialing down the chronic irritation that can bring the healing process to a grinding halt.
By creating this ideal healing environment, SoftWave perfectly prepares the tissue to welcome and work with the cells introduced during stem cell therapy for pain.
This synergistic effect is key. SoftWave doesn't replace stem cell therapy; it enhances it. By preparing the site and calling in local reinforcements, it ensures the specialized "repair crew" can work more effectively, leading to faster and more complete recovery.
The Power of a Combined Approach
Putting these two therapies together gives us a much more robust strategy for tackling chronic pain. The SoftWave treatment acts as a biological primer, getting the healing process fired up before the main event even begins. This ensures the joint or tissue is already in a pro-healing state, ready to make the most of the incoming stem cells.
This combination is especially effective for stubborn, long-standing injuries where poor circulation and chronic inflammation have become major roadblocks. For a deeper look at how this works, you can explore our detailed article on how SoftWave reduces inflammation and promotes healing.
Ultimately, integrating technologies like SoftWave represents a more complete way of thinking about regenerative medicine. It’s about using every tool at our disposal to support and amplify your body’s incredible capacity to heal itself, which translates to better outcomes and more lasting relief from pain.
Why Regenerative Medicine Is a Safer Path Forward
The search for real, lasting pain relief has never been more critical. For a long time, the go-to solution for severe pain was opioid medication—a class of drugs that often comes with a steep price. They might quiet the pain for a little while, but they do it by just masking the signals, all while the original injury is left to get worse.
This approach often kicks off a dangerous cycle. As your body gets used to the drug, you need higher and higher doses to get the same effect, which dramatically increases the risk of dependency and a host of serious side effects. Regenerative medicine, especially stem cell therapy for pain, offers a totally different—and much safer—way forward. It's a path that focuses on healing, not just silencing symptoms.
Instead of flooding your system with powerful synthetic chemicals, this method uses your body’s own natural building blocks to fix the root cause of the pain. It’s a complete shift in thinking, moving from symptom management to true, lasting restoration.
Moving Beyond the Risks of Opioids
So, how do opioids work? They latch onto receptors in your brain and basically tell them to ignore pain signals. They're an outside force that interrupts your body’s internal communication, but they don’t actually do anything to heal the problem. This is what creates such a heavy reliance on an external substance for relief.
Stem cell therapy works on the complete opposite principle. It's an internal, cooperative process that works with your body, not against it. By deploying cells that reduce inflammation and start rebuilding damaged tissue, it helps resolve the very issue that's sending out pain signals in the first place.
This approach is inherently safer because it taps into the body's natural toolkit for healing. There's no risk of dependency, no mind-altering side effects, and no vicious cycle of needing more and more just to get by.
The core difference is simple: Opioids are a temporary patch that hides the problem, while stem cell therapy is a long-term solution that aims to fix it. This distinction is crucial for anyone seeking lasting well-being.
A Focus on Functional Healing
The real goal of regenerative medicine isn’t just to make you feel better; it’s to help you actually get better. The ultimate measure of success is getting your function back. It means being able to jump back into the activities you love without being held back by chronic pain or tied to a daily medication schedule.
This forward-thinking strategy is right in line with a major public health priority: finding meaningful, non-addictive ways to manage pain. It's such a big deal that significant federally funded research is now dedicated to advancing stem cell therapies as a real alternative to opioids.
For example, in late 2022, the Cleveland Clinic received a $5.5 million grant from the National Institutes of Health to develop a stem cell therapy for a severe chronic pain condition. You can read more about the advancements in stem cell research for pain relief to see just how quickly this field is moving.
By focusing on repairing tissue and restoring mobility, this approach paves the way for a more sustainable, active future. This commitment to healing from within is a cornerstone of modern integrative healthcare solutions. It's a responsible, empowering path forward that offers genuine hope for long-term relief without the devastating risks of dependency.
Answering Your Questions About Stem Cell Therapy
It’s completely normal to have questions, even after digging into the science. When you’re thinking about a new way to approach your health, feeling informed is what gives you the confidence to move forward. The world of regenerative medicine is full of exciting possibilities, and our job is to give you clear, straightforward answers.
This section is all about tackling the most common questions we hear about stem cell therapy for pain. By getting these uncertainties out of the way, we hope to give you the last few pieces of the puzzle so you can make the best choice for yourself.
How Long Does It Take to See Results?
This is one of the biggest questions we get, and the answer really shows the difference between a quick fix and true, lasting healing. While some people do report feeling less inflammation and pain within the first few weeks, the real regenerative work is happening on a much longer timeline.
Your body needs time to put those new cells to work repairing and rebuilding damaged tissue. The most significant, lasting improvements typically show up between three to six months after the procedure. It’s a process that requires patience, but that timeline reflects genuine biological repair, not just masking symptoms.
Is the Stem Cell Procedure Painful?
We do everything we can to make the treatment as comfortable as possible. The procedure itself is minimally invasive, and we always use a local anesthetic to completely numb the area we’re working on. Most people tell us they feel little to no discomfort at all during the injections.
After the procedure, it's normal to feel some mild soreness or swelling where the injection was done. This is actually a great sign—it means your body's powerful healing response has been activated and the repair process is officially underway.
That temporary soreness is a lot like how you might feel after a flu shot or a tough workout. It usually fades on its own within a few days and is easily managed with some ice and rest.
How Do I Know If I Am a Good Candidate?
Figuring out if this is the right path for you is the most important step in this whole journey. The only way to know for sure is to sit down for a detailed, one-on-one consultation with a qualified provider.
Generally, the ideal candidates for stem cell therapy for pain are people who:
- Are dealing with chronic pain from degenerative conditions like osteoarthritis.
- Have soft tissue injuries (like tendon or ligament tears) that just haven’t healed with more conservative treatments.
- Are in good overall health and are looking for a way to avoid more invasive options like major surgery.
The evaluation involves a deep dive into your medical history, a physical exam, and a close look at any imaging you have, like X-rays or an MRI. This comprehensive assessment ensures that the therapy is not only a good fit for your specific condition but also has the absolute best chance of success.
Ready to discover if regenerative medicine is the right next step for you? At First Steps Chiropractic, we combine advanced therapies with personalized care to help you get back to the life you love. Schedule your complimentary consultation today!